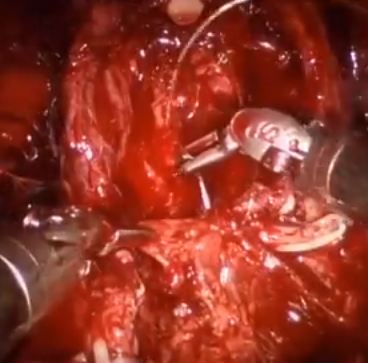
Video: Posterior Muscolofascial Reconstruction after RP
Posterior musculofascial reconstruction after radical prostatectomy: an updated systematic review and a meta-analysis
*, *, †, *, Elisa De Lorenzis*, *, *, *, ‡, §, §, ¶, ¶ and *¶
*Department of Urology, Fondazione IRCCS Ca’ Granda-Ospedale Maggiore Policlinico, University of Milan, Milan, Italy, †DMS StatLab, Data Methods and Systems Statistical Laboratory, University of Brescia, Brescia, Italy, ‡OLV Robotic Surgery Institute, Aalst, Belgium, §Martini Clinic Prostate Cancer Center, University Clinic Eppendorf, Hamburg, Germany, and ¶Global Robotics Institute, Florida Hospital-Celebration Health Celebration, University of Central Florida School of Medicine, Orlando, FL, USA
To evaluate the influence of posterior musculofascial plate reconstruction (PR) on early return of continence after radical prostatectomy (RP); an updated systematic review of the literature. A systematic review of the literature was performed in June 2015, following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement and searching Medline, Embase, Scopus and Web of Science databases. We searched the terms posterior reconstruction prostatectomy, double layer anastomosis prostatectomy across the ‘Title’ and ‘Abstract’ fields of the records, with the following limits: humans, gender (male), and language (English). The authors reviewed the records to identify studies comparing cohorts of patients who underwent RP with or without restoration of the posterior aspect of the rhabdosphincter. A meta-analysis of the risk ratios estimated using data from the selected studies was performed. In all, 21 studies were identified, including three randomised controlled trials. The overall analysis of comparative studies showed that PR improved early continence recovery at 3–7, 30, and 90 days after catheter removal, while the continence rate at 180 days was statistically but not clinically affected. Statistically significantly lower anastomotic leakage rates were described after PR. There were no significant differences for positive surgical margins rates or for complications such as acute urinary retention and bladder neck stricture. The analysis confirms the benefits at 30 days after catheter removal already discussed in the review published in 2012, but also shows a significant advantage in terms of urinary continence recovery in the first 90 days. A multicentre prospective randomised controlled trial is currently being conducted in several institutions around the world to better assess the effectiveness of PR in facilitating an earlier recovery of postoperative urinary continence.