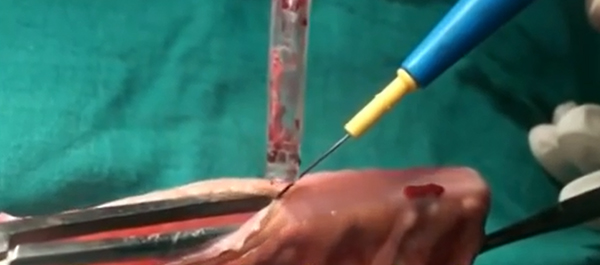
Video: Orthotopic neobladder reconstruction by sigmoid colon
Prospective comparison of quality-of-life outcomes between ileal conduit urinary diversion and orthotopic neobladder reconstruction after radical cystectomy: a statistical model
OBJECTIVE
• To conduct a prospective comparison of quality-of-life (QoL) outcomes in patients who underwent ileal conduit (IC) urinary diversion with those who underwent orthotopic neobladder (ONB) reconstruction after radical cystectomy for invasive bladder cancers.
PATIENTS AND METHODS
• Between January 2007 and December 2012, 227 patients underwent radical cystectomy and either IC urinary diversion or ONB (sigmoid or ileal) reconstruction.
• Contraindications for ON were impaired renal function (serum creatinine >2 mg/dL), chronic inflammatory bowel disease, previous bowel resection and tumour involvement at the bladder neck/prostatic urethra. Patients who did not have these contraindications chose to undergo either IC or ONB reconstruction, after impartial counselling.
• Baseline characteristics, including demographic profile, body mass index, comorbidities, histopathology of the cystoprostatectomy (with lymph nodes) specimen, pathological tumour stage, postoperative complications, adjuvant therapy and relapse, were recorded and compared.
• The European Organization for Research and Treatment of Cancer QoL questionnaire C30 version 3 was used to analyse QoL before surgery and 6, 12 and 18 months after surgery.
RESULTS
• Of the 227 patients, 28 patients in the IC group and 35 in the ONB group were excluded. The final analysis included 80 patients in the IC and 84 in the ONB group.
• None of the baseline characteristics were significantly different between the groups, except for age, but none of the baseline QoL variables were found to be correlated with age.
• In the preoperative phase, there were no significant differences in any of the QoL domains between the IC or the ONB groups. At 6, 12 and 18 months in the postoperative period, physical functioning (P < 0.001, P < 0.001 and P = 0.001, respectively), role functioning (P = 0.01, P = 0.01 and P = 0.003, respectively), social functioning (P = 0.01, P = 0.01 and P = 0.01, respectively) and global health status/QoL (P < 0.001, P < 0.001 and P = 0.002, respectively) were better in patients in the ONB group than in those in the IC group and the differences were significant.
• The financial burden related to bladder cancer treatment was significantly lower in the ONB group than in the IC group at 6, 12 and 18 months of follow-up (P = 0.05, P = 0.05 and P = 0.005, respectively)
CONCLUSIONS
• ONB is better than IC in terms of physical functioning, role functioning, social functioning, global health status/QoL and financial expenditure.
• ONB reconstruction provides better QoL outcomes than does IC urinary diversion.