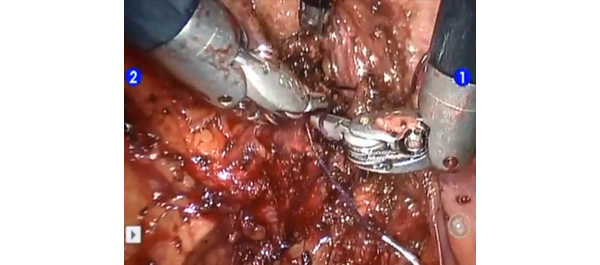
Video: Is LESS more when it comes to nephroureterectomy?
Laparoendoscopic single-site nephroureterectomy for upper urinary tract urothelial carcinoma: outcomes of an international multi-institutional study of 101 patients
Sung Yul Park, Koon Ho Rha1, Riccardo Autorino2, Ithaar Derweesh3, Evangelos Liastikos4, Yao Chou Tsai5, Ill Young Seo6, Ugo Nagele7, Aly M. Abdel-Karim8, Thomas Herrmann9, Deok Hyun Han10, Soroush Rais-Bahrami11, Seung Wook Lee, Kyu Shik Kim, Paolo Fornara12, Panagiotis Kallidonis4, Christopher Springer12, Salah Élsalmy8, Shih-Chieh Jeff Chueh13, Chen-Hsun Ho14, Kamol Panumatrassamee2, Ryan Kopp3, Jens-Uwe Stolzenburg15, Lee Richstone11, Jae Hoon Chung, Tae Young Shin1, Francesco Greco12 and Jihad H. Kaouk2
Department of Urology, Hanyang University College of Medicine, Seoul, Korea, 1Department of Urology, Yonsei University College of Medicine, Seoul, Korea, 2Glickman Urological & Kidney Institute, Cleveland Clinic, Cleveland, OH, USA, 3Division of Urology, University of California San Diego, La Jolla, CA, USA, 4Department of Urology, School of Medicine, University of Patras, Patras, Greece, 5Division of Urology, Buddhist Tzu Chi General Hospital, TaipeiBranch, Taipei, Taiwan, 6Department of Urology, Wonkwang University School of Medicine and Hospital, Iksan, Korea, 7Department of Urology, LKH, Hall in Tirol, Austria, 8Department of Urology, Alexandria University, Alexandria, Egypt, 9Department of Urology, Hannover Medical School, Hannover, Germany, 10Department of Urology, Samsung Medical Center, Sungkyunkwan University, Seoul, Korea, 11The Arthur Smith Institute for Urology, Hofstra North Shore-LIJ School of Medicine, New Hyde Park, NY, USA, 12Department of Urology and Kidney Transplantation, Martin-Luther-University, Halle/Saale, Germany, 13Cleveland Clinic Urology Charleston Office, Charleston, WV, USA, 14Division of Urology, National Taiwan University Hospital, Taipei, Taiwan, 15Department of Urology, University of Leipzig, Leipzig, Germany
OBJECTIVE
• To report a large multi-institutional series of laparoendoscopic single-site (LESS) nephroureterectomy (NU).
MATERIALS AND METHODS
• Data on all cases of LESS-NU performed between 2008 and 2012 at 15 institutions were retrospectively gathered.
• The main demographic data and perioperative outcomes were analysed.
RESULTS
• The study included 101 patients whose mean (sd) age was 66.4 (9.9) years and mean (sd) body mass index was 24.8 (4) kg/m2, and of whom 29.7% had undergone previous abdominal/pelvic surgery.
• The mean (sd) operating time was 221.4 (73.7) min, estimated blood loss 231.7 (348.0) mL.
• A robot-assisted LESS technique was applied in 25.7% of cases. An extra trocar was inserted in 28.7% of cases to complete the procedure. Conversion to open surgery was necessary in three cases (3.0%). There was no bladder cuff excision in 20.8% of cases, and excision was carried out using a variety of techniques in the remaining cases.
• Six intra-operative complications occurred (5.9%). The mean (sd) length of hospital stay was 6.3 (3.5) days. The overall postoperative complication rate was 10.0%, and most of the complications were low grade (Clavien grades 1 and 2).
• The mean tumour size was 3.1 (1.9) cm. Pathological staging was pTis in two patients, pTa in 12 patients, pT1 in 42 patients, pT2 in 20 patients, pT3 in 23 patients and pT4 in two patients. Pathological grade was high in 71 and low in 30 patients.
• At a mean follow-up of 14 months, six patients (5.9%) had died. Disease recurrence (including distant and bladder recurrence) was detected in 22.8% of patients, with a mean time to recurrence of 11.5 months.
CONCLUSIONS
• This study reports the largest multi-institutional experience of LESS-NU to date.
• Peri-operative outcomes mirror those of published standard laparoscopy series.
• Despite encouraging early findings, longer follow-up is needed to determine the oncological efficacy of the procedure.