Article of the month: MRI and active surveillance for prostate cancer
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Dr. Hyun M. Lee discussing his paper.
If you only have time to read one article this week, it should be this one.
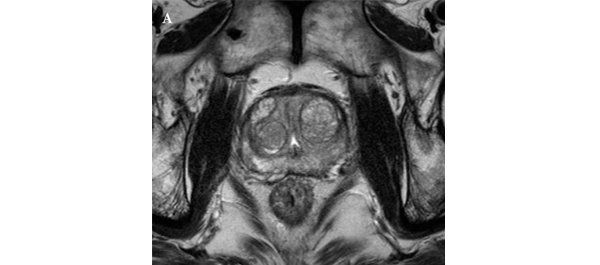
Role of multiparametric 3.0-Tesla magnetic resonance imaging in patients with prostate cancer eligible for active surveillance
Bong H. Park, Hwang G. Jeon, Seol H. Choo, Byong C. Jeong, Seong I. Seo, Seong S. Jeon, Han Y. Choi and Hyun M. Lee
Department of Urology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
Current address: Bong H. Park, Department of Urology, Incheon St. Mary’s Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea
OBJECTIVE
• To evaluate predictors of more aggressive disease and the role of multiparametric 3.0-T magnetic resonance imaging (MRI) in selecting patients with prostate cancer for active surveillance (AS).
PATIENTS AND METHODS
• We retrospectively assessed 298 patients with prostate cancer who met the Prostate Cancer Research International: Active Surveillance (PRIAS) criteria, defined as T1c/T2, PSA level of ≤10 ng/mL, PSA density (PSAD) of <0.2 ng/mL2, Gleason score <7, and one or two positive biopsy cores.
• All patients underwent preoperative MRI, including T2-weighted, diffusion-weighted, and dynamic contrast-enhanced imaging, as well as radical prostatectomy (RP) between June 2005 and December 2011.
• Imaging results were correlated with pathological findings to evaluate the ability of MRI to select patients for AS.
RESULTS
• In 35 (11.7%) patients, no discrete cancer was visible on MRI, while in the remaining 263 (88.3%) patients, a discrete cancer was visible.
• Pathological examination of RP specimens resulted in upstaging (>T2) in 21 (7%) patients, upgrading (Gleason score >6) in 136 (45.6%), and a diagnosis of unfavourable disease in 142 (47.7%) patients.
• The 263 patients (88.3%) with visible cancer on imaging were more likely to have their cancer status upgraded (49.8% vs 14.3%) and be diagnosed with unfavourable disease (52.1% vs 14.3%) than the 35 patients (11.7%) with no cancer visible upon imaging, and these differences were statistically significant (P < 0.001 for all).
• A visible cancer lesion on MRI, PSAD, and patient age were found to be predictors of unfavourable disease in multivariate analysis.
CONCLUSION
• MRI can predict adverse pathological features and be used to assess the eligibility of patients with prostate cancer for AS.