Video: Combination of mpMRI and TTMB of the prostate to identify candidates for hemi-ablative FT
Combination of multi-parametric magnetic resonance imaging (mp-MRI) and transperineal template-guided mapping biopsy (TTMB) of the prostate to identify candidates for hemi-ablative focal therapy
OBJECTIVE
To evaluate the accuracy of combined multiparametric magnetic resonance imaging (mpMRI) and transperineal template-guided mapping biopsy (TTMB) for identifying lobes with significant prostate cancer (PCa) for the application of hemi-ablative focal therapy (FT).
PATIENTS AND METHODS
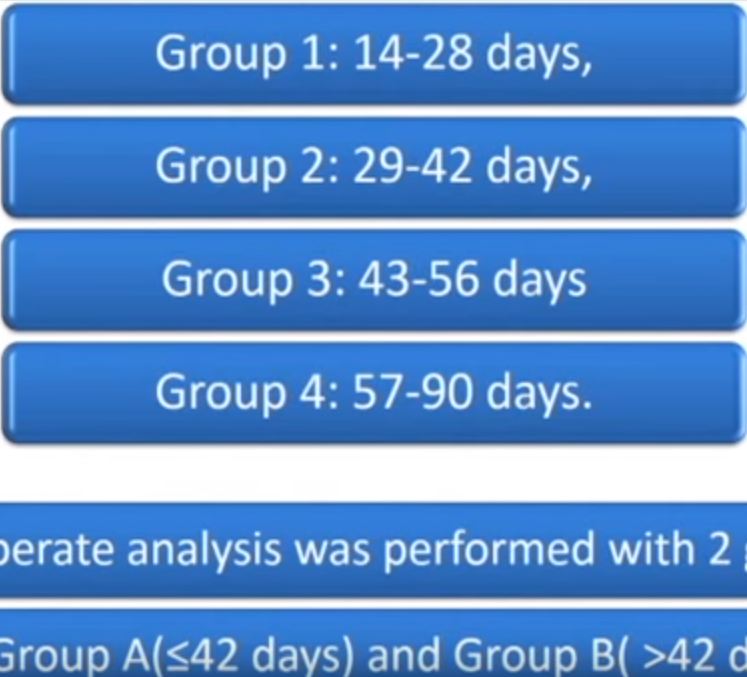
From January 2012 to January 2014, 89 consecutive patients, aged ≥40 years, with a PSA level ≤15 ng/mL, underwent in sequential order: mpMRI, TTMB and radical prostatectomy (RP) at a single centre. Analysis was performed on 50 patients who met consensus guidelines for FT. Lobes were stratified into lobes with significant cancer (LSC), lobes with insignificant cancer and lobes with no cancer. Using histopathology at RP, the predictive performance of combined mpMRI + TTMB in identifying LSC was evaluated.
RESULTS
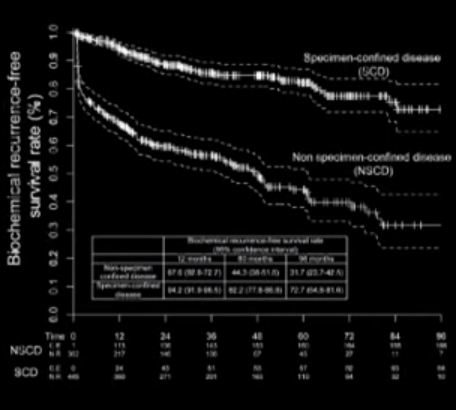
The sensitivity, specificity and positive predictive value for mpMRI + TTMB for LSC were 97, 61 and 83%, respectively. The negative predictive value (NPV), the primary variable of interest, for mpMRI + TTMB for LSC was 91%. Of the 50 patients, 21 had significant unilateral disease on mpMRI + TTMB. Two of these 21 patients had significant bilateral disease on RP not identified on mpMRI + TTMB.
CONCLUSIONS
In the selection of candidates for FT, a combination of mpMRI and TTMB provides a high NPV in the detection of LSC.