Posts
Residents’ podcast: MIMIC Study
Part of the BURST/BJUI Podcast Series
Mr Chuanyu Gao is a Core Surgical Trainee in KSS Deanery. He graduated from UCL Medical School and obtained his iBSc in Surgical Sciences before completing his Academic Foundation Years in East of England Foundation School. Chuanyu first became involved with BURST on the MIMIC Study as an international site coordinator and has been part of the BURST committee ever since.
Factors associated with spontaneous stone passage in a contemporary cohort of patients presenting with acute ureteric colic: results from the Multi‐centre cohort study evaluating the role of Inflammatory Markers In patients presenting with acute ureteric Colic (MIMIC) study
Taimur T. Shah*†‡§, Chuanyu Gao*, Max Peters¶, Todd Manning**, Sophia Cashman*, Arjun Nambiar*, Marcus Cumberbatch*††, Ben Lamb*, Anthony Peacock‡‡, Marieke J. Van Son¶, Peter S. N. van Rossum¶, Robert Pickard§§, Paul Erotocritou¶¶, Daron Smith***, Veeru Kasivisvanathan*‡ and British Urology Researchers in Surgical Training (BURST) Collaborative MIMIC Study Group
*British Urology Researchers in Surgical Training (BURST), London, UK, †Division of Surgery and Cancer, Imperial College London, ‡Division of Surgery and Interventional Science, University College London, §Charing Cross Hospital, Imperial Health NHS Trust, London, UK, ¶Department of Radiation Oncology, Cancer Center, University Medical Center Utrecht, Utrecht, The Netherlands, **Australian Young Urology Researchers Organisation (YURO), Heidelberg, Victoria, Australia, ††Academic Urology Unit, University of Sheffield, Sheffield, ‡‡Information Services Division, University College London (UCL), London, §§Department of Urology, Newcastle University, Newcastle, UK, ¶¶Department of Urology, Whittington Hospital, and ***Department of Urology, UCL Hospital, London, UK
Article of the week: Management of large renal stones with super‐mini percutaneous nephrolithotomy: an international multicentre comparative study
Every week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
There is also a visual abstract created by Cora Griffin from King’s College London.
If you only have time to read one article this week, we recommend this one.
Management of large renal stones with super-mini percutaneous nephrolithotomy: an international multicentre comparative study
Yang Liu*, Chao Cai*, Albert Aquino†, Shabir Al-Mousawi‡, Xuepei Zhang§, Simon K.S. Choong¶, Xiang He**, Xianming Fan††, Bin Chen‡‡, Jianhua Feng§§, Xuhui Zhu¶¶, Abdulla Al-Naimi***, Houping Mao†††, Huilong Tang‡‡‡, Dayong Jin§§§, Xiancheng Li¶¶¶, Fenghong Cao****, Hua Jiang††††, Yongfu Long‡‡‡‡, Wei Zhang§§§§, Gang Wang¶¶¶¶, Zihao Xu*, Xin Zhang*, Shanfeng Yin* and Guohua Zeng*
*Department of Urology, Guangdong Key Laboratory of Urology, Minimally Invasive Surgery Center, The First Affiliated Hospital of Guangzhou Medical University, Guangzhou, China, †Department of Urology, Jose R. Reyes Memorial Medical Center, Manila, Philippines, ‡Division of Urology, SABAH ALAHMAD Urology Center, Ministry of Health, Al-Amiri Hospital, Kuwait City, Kuwait, §Department of Urology, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, China, ¶Institute of Urology, University College London Hospitals, London, UK, **Department of Urology, Zhejiang Provincial People’s Hospital, People’s Hospital of Hangzhou Medical College, Hangzhou, ††Department of Urology, The Third Affiliated Hospital of Xiamen, The Third Affiliated Hospital of Fujian University of Traditional Chinese Medicine, ‡‡Department of Urology, The Affiliated Hospital of Xiamen University, Xiamen, §§Department of Urology, Longgang District Central Hospital, Shenzhen, ¶¶Department of Urology, Beijing Chaoyang Hospital, Affiliated to Capital Medical University, Beijing, China, ***Department of Urology, Hamad Medical Corporation, Doha, Qatar, †††Department of Urology, First Affiliated Hospital of Fujian Medical University, Fuzhou, ‡‡‡Department of Urology, The First Hospital of Hunan University of Traditional Chinese Medicine, Changsha, §§§Department of Urology, Liaoyuan City Central Hospital, Liaoyuan, ¶¶¶Department of Urology, Second Affiliated Hospital of Dalian Medical University, Dalian, ****Department of Urology, North China University of Science and Technology Affiliated Hospital, Tangshan, ††††Department of Urology, Zhongda Hospital Southeast Hospital, Nanjing, ‡‡‡‡Department of Urology, Central Hospital of Shaoyang, Shaoyang, §§§§Department of Urology, The First Affiliated Hospital of Nanjing Medical University, Nanjing, and ¶¶¶¶Department of Urology, National Urological Cancer Center, Institute of Urology, Peking University First Hospital, Peking University, Beijing, China
Abstract
Objectives
To comparatively evaluate the clinical outcomes of super‐mini percutaneous nephrolithotomy (SMP) and mini‐percutaneous nephrolithotomy (Miniperc) for treating urinary tract calculi of >2 cm.
Patients and Methods
An international multicentre, retrospective cohort study was conducted at 20 tertiary care hospitals across five countries (China, the Philippines, Qatar, UK, and Kuwait) between April 2016 and May 2019. SMP and Miniperc were performed in 3525 patients with renal calculi with diameters of >2 cm. The primary endpoint was the stone‐free rate (SFR). The secondary outcomes included: blood loss, operating time, postoperative pain scores, auxiliary procedures, complications, tubeless rate, and hospital stay. Propensity score matching analysis was used to balance the selection bias between the two groups.
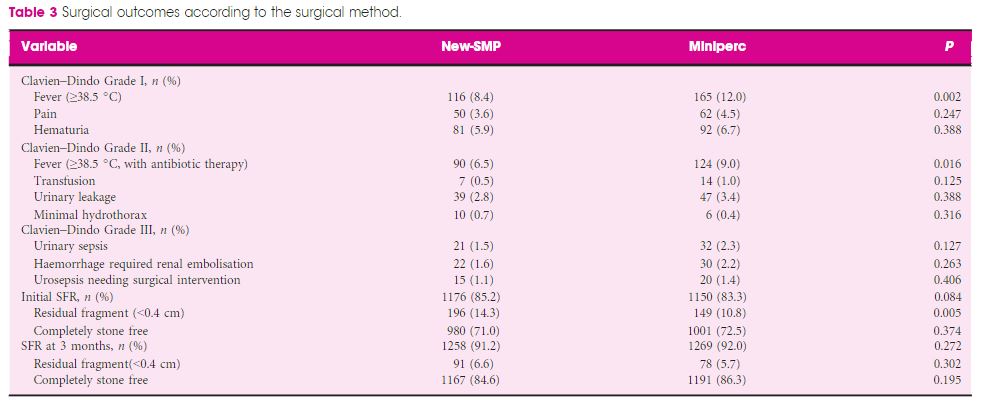
Results
In all, 2012 and 1513 patients underwent SMP and Miniperc, respectively. After matching, 1380 patients from each group were included for further analysis. Overall, there was no significant difference in the mean operating time or SFR between the two groups. However, the hospital stay and postoperative pain score were significantly in favour of SMP (both P < 0.001). The tubeless rate was significantly higher in the SMP group (72.6% vs 57.8%, P < 0.001). Postoperative fever was much more common in the Miniperc group (12.0% vs 8.4%, P = 0.002). When the patients were further classified into three subgroups based on stones diameters (2–3, 3–4, and >4 cm). The advantages of SMP were most obvious in the 2–3 cm stone group and diminished as the size of the stone increased, with longer operating time in the latter two subgroups. Compared with Miniperc, the SFR of SMP was comparable for 3–4 cm stones, but lower for >4 cm stones. There was no statistical difference in blood transfusions and renal embolisations between the two groups.
Conclusions
Our data showed that SMP is an ideal treatment option for stones of <4 cm and is more efficacious for stones of 2–3 cm, with lesser postoperative fever, blood loss, and pain compared to Miniperc. SMP was less effective for stones of >4 cm, with a prolonged operating time.
Article of the week: Deep learning computer vision algorithm for detecting kidney stone composition
Every week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
If you only have time to read one article this week, we recommend this one.
Deep learning computer vision algorithm for detecting kidney stone composition
Kristian M. Black*, Hei Law†, Ali Aldoukhi*, Jia Deng† and Khurshid R. Ghani*
*Department of Urology, University of Michigan, Ann Arbor, MI, and †Department of Computer Science, Princeton University, Princeton, NJ, USA
Abstract
Objectives
To assess the recall of a deep learning (DL) method to automatically detect kidney stones composition from digital photographs of stones.
Materials and Methods
A total of 63 human kidney stones of varied compositions were obtained from a stone laboratory including calcium oxalate monohydrate (COM), uric acid (UA), magnesium ammonium phosphate hexahydrate (MAPH/struvite), calcium hydrogen phosphate dihydrate (CHPD/brushite), and cystine stones. At least two images of the stones, both surface and inner core, were captured on a digital camera for all stones. A deep convolutional neural network (CNN), ResNet‐101 (ResNet, Microsoft), was applied as a multi‐class classification model, to each image. This model was assessed using leave‐one‐out cross‐validation with the primary outcome being network prediction recall.
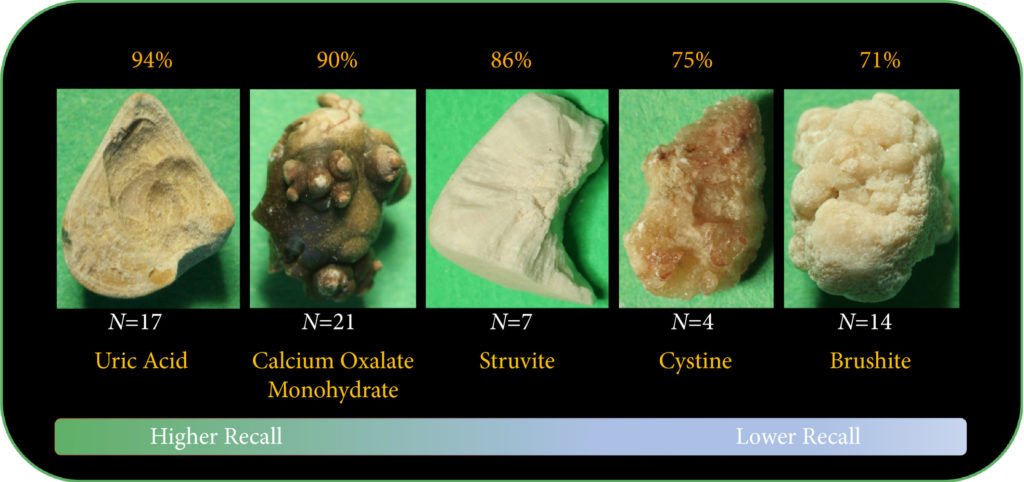
Results
The composition prediction recall for each composition was as follows: UA 94% (n = 17), COM 90% (n = 21), MAPH/struvite 86% (n = 7), cystine 75% (n = 4), CHPD/brushite 71% (n = 14). The overall weighted recall of the CNNs composition analysis was 85% for the entire cohort. Specificity and precision for each stone type were as follows: UA (97.83%, 94.12%), COM (97.62%, 95%), struvite (91.84%, 71.43%), cystine (98.31%, 75%), and brushite (96.43%, 75%).
Conclusion
Deep CNNs can be used to identify kidney stone composition from digital photographs with good recall. Future work is needed to see if DL can be used for detecting stone composition during digital endoscopy. This technology may enable integrated endoscopic and laser systems that automatically provide laser settings based on stone composition recognition with the goal to improve surgical efficiency.
Article of the Month: SMP vs retrograde intrarenal surgery for the treatment of 1–2 cm lower‐pole renal calculi: an international multicentre RCT
Every month, the Editor-in-Chief selects an Article of the Month from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation. There is also a video, provided by the authors, showing SMP.
If you only have time to read one article this week, it should be this one.
Super‐mini percutaneous nephrolithotomy (SMP) vs retrograde intrarenal surgery for the treatment of 1–2 cm lower‐pole renal calculi: an international multicentre randomised controlled trial
Guohua Zeng* , Tao Zhang* , Madhu Agrawal†, Xiang He‡, Wei Zhang§, Kefeng Xiao¶, Hulin Li**, Xuedong Li††, Changbao Xu‡‡, Sixing Yang§§, Jean J. de la Rosette¶¶***, Junhong Fan*, Wei Zhu* and Kemal Sarica†††
Department of Urology *Minimally Invasive Surgery Center, The First Affiliated Hospital of Guangzhou Medical University, **Guangdong Key Laboratory of Urology, ZhuJiang Hospital of Southern Medical University, Guangzhou, ‡Zhejiang Provincial People’s Hospital, Zhejiang, §The First Affiliated Hospital With Nanjing Medical University, Nanjing, ¶Shenzhen People’s Hospital, Shenzhen, ††The Second Affiliated Hospital of Harbin Medical University, Harbin, ‡‡The Second Affiliated Hospital of Zhengzhou University, Zhengzhou, §§Renmin Hospital of Wuhan University, Wuhan, China, †Centre for Minimally Invasive Endourology, Global Rainbow Healthcare, Agra, India, ¶¶Istanbul Medipol University, Istanbul, Turkey, ***AMC University Hospital, Amsterdam, The Netherlands, and †††Dr. Lutfi Kirdar Kartal Research and Training Hospital, Istanbul, Turkey
Abstract
Objectives
To compare the safety and effectiveness of super‐mini‐percutaneous nephrolithotomy (SMP) and retrograde intrarenal surgery (RIRS) for the treatment of 1–2 cm lower‐pole renal calculi (LPC).
Patients and Methods
An international multicentre, prospective, randomised, unblinded controlled study was conducted at 10 academic medical centres in China, India, and Turkey, between August 2015 and June 2017. In all, 160 consecutive patients with 1–2 cm LPC were randomised to receive SMP or RIRS. The primary endpoint was stone‐free rate (SFR). Stone‐free status was defined as no residual fragments of ≥0.3 cm on plain abdominal radiograph of the kidneys, ureters and bladder, and ultrasonography at 1‐day and on computed tomography at 3‐months after operation. Secondary endpoints included blood loss, operating time, postoperative pain scores, auxiliary procedures, complications, and hospital stay. Postoperative follow‐up was scheduled at 3 months. Analysis was by intention‐to‐treat. The trial was registered at https://clinicaltrials.gov/ (NCT02519634).
Results
The two groups had similar baseline characteristics. The mean (sd) stone diameters were comparable between the groups, at 1.50 (0.29) cm for the SMP group vs 1.43 (0.34) cm for the RIRS group (P = 0.214). SMP achieved a significantly better 1‐day and 3‐month SFR than RIRS (1‐day SFR 91.2% vs 71.2%, P = 0.001; 3‐months SFR 93.8% vs 82.5%, P = 0.028). The auxiliary procedure rate was lower in the SMP group. RIRS was found to be superior with lower haemoglobin drop and less postoperative pain. Blood transfusion was not required in either group. There was no significant difference in operating time, hospital stay, and complication rates, between the groups.
Conclusions
SMP was more effective than RIRS for treating 1–2 cm LPC in terms of a better SFR and lesser auxiliary procedure rate. The complications and hospital stay were comparable. RIRS has the advantage of less postoperative pain.
Article of the Week: Antibiotic prophylaxis in ureteroscopic lithotripsy
Every Week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Antibiotic prophylaxis in ureteroscopic lithotripsy: a systematic review and meta‐analysis of comparative studies
*†‡, §, *†‡, *†‡, *†‡, *†‡, *†‡, *†‡ and *†‡
*Department of Urology, Minimally Invasive Surgery Center, The First Affiliated Hospital of Guangzhou Medical University, Guangzhou, China, †Guangzhou Institute of Urology, Guangzhou, China, ‡Guangdong Key Laboratory of Urology, Guangzhou, China, and §The First Affiliated Hospital of Jinan University, Guangzhou, China
Abstract
Objective
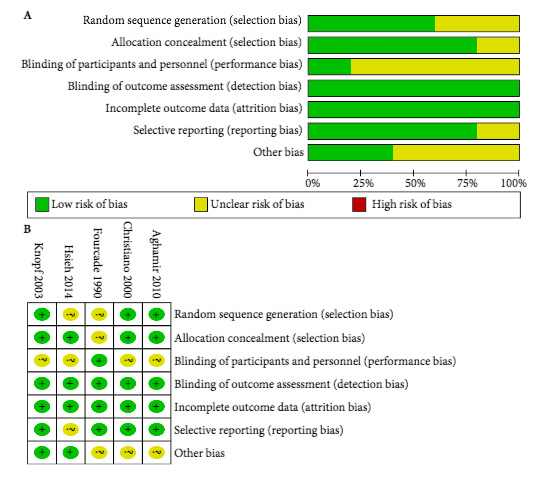
To explore the efficacy of antibiotic prophylaxis and the different strategies used to prevent infection in ureteroscopic lithotripsy (URL) by conducting a systematic review and meta‐analysis.
Materials and Methods
A systematic literature search using Pubmed, Embase, Medline, the Cochrane Library, and the Chinese CBM, CNKI and VIP databases was performed to find comparative studies on the efficacy of different antibiotic prophylaxis strategies in URL for preventing postoperative infections. The last search was conducted on 25 June 2017. Summarized unadjusted odds ratios (ORs) with 95% confidence intervals (CIs) were calculated to assess the efficacy of different antibiotic prophylaxis strategies.
Results
A total of 11 studies in 4 591 patients were included in this systematic review and meta‐analysis. No significant difference was found in the risk of postoperative febrile urinary tract infections (fUTIs) between groups with and without antibiotic prophylaxis (OR: 0.82, 95% CI 0.40–1.67; P = 0.59). Patients receiving a single dose of preoperative antibiotics had a significantly lower risk of pyuria (OR: 0.42, 95% CI 0.25–0.69; P = 0.0007) and bacteriuria (OR: 0.25, 95% CI 0.11–0.58; P = 0.001) than those who did not. Intravenous antibiotic prophylaxis was not superior to single‐dose oral antibiotic prophylaxis in reducing fUTI (OR: 1.00, 95% CI 0.26–3.88; P = 1.00).
Conclusions
We concluded that preoperative antibiotic prophylaxis did not lower the risk of postoperative fUTI, but a single dose could reduce the incidence of pyuria or bacteriuria. A single oral dose of preventive antibiotics is preferred because of its cost‐effectiveness. The efficacy of different types of antibiotics and other strategies could not be assessed in our meta‐analysis. Randomized controlled trials with a larger sample size and more rigorous study design are needed to validate these conclusions.
Article of the Month: Surgical outcomes of PCNL and results of stone analysis
Every Month the Editor-in-Chief selects an Article of the Month from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Surgical outcomes of percutaneous nephrolithotomy in 3402 patients and results of stone analysis in 1559 patients
*, *, *, *, * and †
*Departments of Urology, and †Pathology, Sindh Institute of Urology and Transplantation, Civil Hospital, Karachi, Pakistan
Abstract
Objective
To report our experience of a series of percutaneous nephrolithotomy (PCNL) procedures in a single centre over 18 years in terms of patient and stone characteristics, indications, stone clearance and complications, along with the results of chemical analysis of stones in a subgroup.
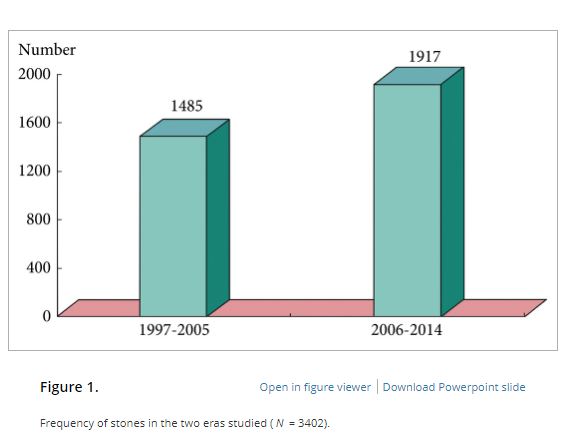
Patients and Methods
We retrospectively analysed the outcomes of PCNL in 3402 patients, who underwent the procedure between 1997 and 2014, obtained from a prospectively maintained database. Data analysis included patients’ age and sex, laboratory investigations, imaging, punctured calyx, duration of operation, volume of irrigation fluid, radiation exposure time, blood transfusion, complications and stone-free status at 1-month follow-up. For the present analysis, outcomes in relation to complications and success were divided in two eras, 1997–2005 and 2006–2014, to study the differences.
Results
Of the 3402 patients, 2501 (73.5%) were male and 901 (26.5%) were female, giving a male:female ratio of 2.8:1. Staghorn (partial or complete) calculi were found in 27.5% of patients, while 72.5% had non-staghorn calculi. Intracorporeal energy sources used for stone fragmentation included ultrasonography in 917 patients (26.9%), pneumatic lithoclast in 1820 (53.5%), holmium laser in 141 (4.1%) and Lithoclast® master in 524 (15.4%). In the majority of patients (97.4%) a 18–22-F nephrostomy tube was placed after the procedure, while 69 patients (2.03%) underwent tubeless PCNL. The volume of the irrigation fluid used ranged from 7 to 37 L, with a mean of 28.4 L. The stone-free rate after PCNL in the first era studied was 78%, vs 83.2% in the second era, as assessed by combination of ultrasonography and plain abdominal film of the kidney, ureter and bladder. The complication rate in the first era was 21.3% as compared with 10.3% in the second era, and this difference was statistically significant. Stone analysis showed pure stones in 41% and mixed stones in 58% of patients. The majority of stones consisted of calcium oxalate.
Conclusions
This is the largest series of PCNL reported from any single centre in Pakistan, where there is a high prevalence of stone disease associated with infective and obstructive complications, including renal failure. PCNL as a treatment method offers an economic and effective option in the management of renal stone disease with acceptable stone clearance rates in a resource-constrained healthcare system.
Editorial: Management of urolithiasis in South Asia
The article by Rizvi et al. [1] makes a great read. The authors deserve credit for their work and the data presented. A few points merit mention to summarise and put the article in perspective.
First, the authors present a mammoth database from a public sector hospital in Pakistan. In the initial era, as noted by the authors, they adopted extracorporeal shockwave lithotripsy (ESWL) as their mainstay for treating stones. ESWL as the least invasive, safe and readily available method remained the preferred option initially. However, stones seen in South Asia differ from those in the West. In this geographical area, the stone bulk is large and often not amenable to ESWL. In the subsequent period, the authors changed to percutaneous surgery. The reason for this shift, apart from large stone burden, may also have been influenced by local facto required to be travelled by patients to reach a healthcare facility and the lack of resources and infrastructure in remote locations. In such situations, the treatment option that offers rapid, safe, and efficacious results would be preferred. These criteria are fulfilled with the percutaneous approach to renal stones and this is what the authors did!
Second, it is worthwhile noting that that the need for embolisation and/or nephrectomy is a miniscule number in this series [1]. This emphasises the importance of the basic tenet in percutaneous renal surgery that a perfect initial access is the secret to successful percutaneous removal of stones. It should be noted that in this large series the complications across all Clavien–Dindo complication grades reduced as the authors ascended the learning curve.
Third, we feel the major limitation of this study [1] was the means of assessing the stone-free rate. The authors used a combination of ultrasonography and plain abdominal radiograph of the kidneys, ureters and bladder. As acknowledged by the authors this could have possibly overestimated the stone-free rates and skewed the data and interpretation. The authors can substantiate these findings in further prospective studies.
Fourth, the paper exemplifies that stone composition, choice of approach, and patient preferences vary from region to region globally. The findings in the study [1] are similar to the results of Desai et al. [2] from India.
Last but not the least, the AUA guidelines [3] state that the optimal strategy for stone management must take into consideration patient health and economic outcomes. Stone-free requirement is global but economic implications are regional. In this context, the treatment options for similar sized stones may vary for a particular patient located in Europe or Asia. Hence, we feel this paper could be considered as a benchmark for future multicentre trials investigating treatment options and strategies for urolithiasis in South Asia.
and
Department of Urology, Muljibhai Patel Urological Hospital, Nadiad, Gujarat, India
References
1 Rizvi SA, Hussain M, Askari SH, Hashmi A, Lal M, Zafar MN. Surgical outcomes of percutaneous nephrolithotomy in 3402 patients and results of stone analysis in 1559 patients from a single centre in Pakistan. BJUInt 2017; 120: 702–9
2 Desai M, Jain P, Ganpule A, Sabnis R, Patel S, Shrivastav P. Developments in technique and technology: the effect on the results of percutaneous nephrolithotomy for staghorn calculi. BJU Int 2009; 104:542–8
3 Assimos D, Krambeck A, Miller NL et al. Surgical management of stones: American Urological Association/Endourological Society Guideline. Available at: https://www.auanet.org/guidelines/surgical-management-of-stones-(aua/endourological-society-guideline-2016). Accessed August 2017