Posts
Residents’ podcast: Artificial intelligence applications in urology
Maria Uloko is a Urology Resident at the University of Minnesota Hospital. In this podcast she is joined by Dr Christopher Weight, an Associate Professor in the Department of Urology at the University of Minnesota. They are discussing a recent BJUI Article of the month:
Current status of artificial intelligence applications in urology and their potential to influence clinical practice
Abstract
Objective
To investigate the applications of artificial intelligence (AI) in diagnosis, treatment and outcome prediction in urologic diseases and evaluate its advantages over traditional models and methods.
Materials and methods
A literature search was performed after PROSPERO registration (CRD42018103701) and in compliance with Preferred Reported Items for Systematic Reviews and Meta‐Analyses (PRISMA) methods. Articles between 1994 and 2018 using the search terms “urology”, “artificial intelligence”, “machine learning” were included and categorized by the application of AI in urology. Review articles, editorial comments, articles with no full‐text access, and nonurologic studies were excluded.
Results
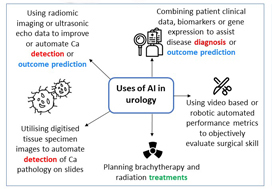
Initial search yielded 231 articles, but after excluding duplicates and following full‐text review and examination of article references, only 111 articles were included in the final analysis. AI applications in urology include: utilizing radiomic imaging or ultrasonic echo data to improve or automate cancer detection or outcome prediction, utilizing digitized tissue specimen images to automate detection of cancer on pathology slides, and combining patient clinical data, biomarkers, or gene expression to assist disease diagnosis or outcome prediction. Some studies employed AI to plan brachytherapy and radiation treatments while others used video-based or robotic automated performance metrics to objectively evaluate surgical skill. Compared to conventional statistical analysis, 71.8% of studies concluded that AI is superior in diagnosis and outcome prediction.
Conclusion
AI has been widely adopted in urology. Compared to conventional statistics AI approaches are more accurate in prediction and more explorative for analyzing large data cohorts. With an increasing library of patient data accessible to clinicians, AI may help facilitate evidence‐based and individualized patient care.
BJUI Podcasts now available on iTunes, subscribe here https://itunes.apple.com/gb/podcast/bju-international/id1309570262
Dr Weight specializes in the surgical treatment of urologic cancers including prostate, bladder, kidney, adrenal, testis and penile cancer. He performs open, endoscopic, laparoscopic, robotic (da Vinci) and retroperineoscopic surgery.
Dr Weight completed his residency training at Cleveland Clinic where he received several awards including the George and Grace Crile Traveling Fellowship Award, the Society of Laparoendoscopic Surgeons Resident Achievement Award and the ASCO Genitourinary Cancer Symposium Merit Award. Dr. Weight then completed a fellowship in Urologic Oncology at Mayo Clinic, where he also completed a Masters degree in Clinical and Translational Research from Mayo Graduate School and was awarded the Mayo Fellows Association Humanitarian Award.
Dr Weight believes that medical research is a key component to offering excellent patient care. His research is focused on improving patient outcomes and the use of artificial intelligence in different urologic applications. He is an author of more than 45 peer-reviewed publications and book chapters and has been invited to speak at regional, national and international conferences.
A taster week in urology and renal transplant in the UK
A taster week is a training opportunity offered to UK doctors in their first two years of clinical practice to try a new specialty. They are an important learning experience for doctors at this stage, who will have experienced working in six different specialties at most. While taster weeks are only five days long, they offer a unique insight into a new specialty, as well as the chance to network with registrars and consultants.
During medical school I was interested in transplantation, as I found the combination between surgery and immunology interesting. This led me to complete a Master of Research in Transplantation while at medical school. During this degree, I looked at urinary tract infection in transplant patients and this started my interest in urology.
In the UK, the majority of trainees enter the field of transplantation following training in General Surgery. In clinical practice, it is good to have urologists with an active interest in Renal Transplantation for the betterment of these patients but there are few centres where this can be learnt. However, the Freeman Hospital in Newcastle, UK offers a one to two-year fellowship in renal transplantation which can be completed at the end of urology training. I contacted one of the urology and renal transplant surgeons and organised a week’s visit to the Freeman Hospital.
During my taster week I had the opportunity to shadow a urology and renal transplant surgeon. I joined urology and transplant ward rounds, including a renal transplant grand round, and I also attended a transplant nephrology clinic where I saw the long-term management of patients who had received kidney transplants. I observed theatre lists in both urology and transplant and saw the wide variety of operations that urology and transplant surgeons are involved in, such as renal access surgery for dialysis and robotic partial nephrectomy for renal cancer.
I also had a chance to attend multi-disciplinary team meetings about new transplant recipients as well as an x-ray imaging meeting concerning live kidney donors.
Speaking to urology and renal transplant surgeons was an invaluable experience and helped me plan the next steps in my career as well as solidify it as a preferred career choice.
The highlight of my taster week was attending regional surgical teaching. I spent a day in one of the few world-class cadaveric training laboratories in the UK and learnt how to perform an orchidopexy for testicular torsion and vascular anastomosis; two operations that are no doubt necessary for a urology and renal transplant surgeon.
I am very glad I completed a taster week in urology and renal transplantation. It allowed me to experience the variety of work involved in this niche specialty. It was an experience that would have only been available much later in my career otherwise, which would be at a point too late for a career change.
by Matthew Byrne
Matthew Byrne recently completed two years as an Academic Foundation Doctor in Cambridge, UK. He graduated MBBS from Newcastle where he also completed a Master of Research in Transplantation. He is now a Urology Clinical Fellow in Cambridge, UK.
Article of the month: Current status of artificial intelligence applications in urology and their potential to influence clinical practice
Every month, the Editor-in-Chief selects an Article of the Month from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an editorial and a visual abstract produced by prominent members of the urological community. These are intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this month, it should be this one.
Current status of artificial intelligence applications in urology and their potential to influence clinical practice
Jian Chen*, Daphne Remulla*, Jessica H. Nguyen*, D. Aastha†, Yan Liu†, Prokar Dasgupta‡ and Andrew J. Hung*
*Catherine & Joseph Aresty Department of Urology, Center for Robotic Simulation & Education, University of Southern California Institute of Urology, †Computer Science Department, Viterbi School of Engineering, University of Southern California, Los Angeles, CA, USA, and ‡Division of Transplantation Immunology and Mucosal Biology, Faculty of Life Sciences and Medicine, Kings College London, London, UK
Abstract
Objective
To investigate the applications of artificial intelligence (AI) in diagnosis, treatment and outcome prediction in urologic diseases and evaluate its advantages over traditional models and methods.
Materials and methods
A literature search was performed after PROSPERO registration (CRD42018103701) and in compliance with Preferred Reported Items for Systematic Reviews and Meta‐Analyses (PRISMA) methods. Articles between 1994 and 2018 using the search terms “urology”, “artificial intelligence”, “machine learning” were included and categorized by the application of AI in urology. Review articles, editorial comments, articles with no full‐text access, and non-urologic studies were excluded.
Results
Initial search yielded 231 articles, but after excluding duplicates and following full‐text review and examination of article references, only 111 articles were included in the final analysis. AI applications in urology include: utilizing radiomic imaging or ultrasonic echo data to improve or automate cancer detection or outcome prediction, utilizing digitized tissue specimen images to automate detection of cancer on pathology slides, and combining patient clinical data, biomarkers, or gene expression to assist disease diagnosis or outcome prediction. Some studies employed AI to plan brachytherapy and radiation treatments while others used video based or robotic automated performance metrics to objectively evaluate surgical skill. Compared to conventional statistical analysis, 71.8% of studies concluded that AI is superior in diagnosis and outcome prediction.
Conclusion
AI has been widely adopted in urology. Compared to conventional statistics AI approaches are more accurate in prediction and more explorative for analyzing large data cohorts. With an increasing library of patient data accessible to clinicians, AI may help facilitate evidence‐based and individualized patient care.
Video: Current status of artificial intelligence applications in urology
Current status of artificial intelligence applications in urology and their potential to influence clinical practice
Abstract
Objective
To investigate the applications of artificial intelligence (AI) in diagnosis, treatment and outcome prediction in urologic diseases and evaluate its advantages over traditional models and methods.
Materials and methods
A literature search was performed after PROSPERO registration (CRD42018103701) and in compliance with Preferred Reported Items for Systematic Reviews and Meta‐Analyses (PRISMA) methods. Articles between 1994 and 2018 using the search terms “urology”, “artificial intelligence”, “machine learning” were included and categorized by the application of AI in urology. Review articles, editorial comments, articles with no full‐text access, and non-urologic studies were excluded.
Results
Initial search yielded 231 articles, but after excluding duplicates and following full‐text review and examination of article references, only 111 articles were included in the final analysis. AI applications in urology include: utilizing radiomic imaging or ultrasonic echo data to improve or automate cancer detection or outcome prediction, utilizing digitized tissue specimen images to automate detection of cancer on pathology slides, and combining patient clinical data, biomarkers, or gene expression to assist disease diagnosis or outcome prediction. Some studies employed AI to plan brachytherapy and radiation treatments while others used video based or robotic automated performance metrics to objectively evaluate surgical skill. Compared to conventional statistical analysis, 71.8% of studies concluded that AI is superior in diagnosis and outcome prediction.
Conclusion
AI has been widely adopted in urology. Compared to conventional statistics AI approaches are more accurate in prediction and more explorative for analyzing large data cohorts. With an increasing library of patient data accessible to clinicians, AI may help facilitate evidence‐based and individualized patient care.
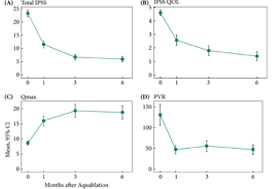
Article of the week: Aquablation for benign prostatic hyperplasia in large prostates: 6‐month results from the WATER II trial
Every week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
We invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Aquablation for benign prostatic hyperplasia in large prostates (80–150 mL): 6‐month results from the WATER II trial
Mihir Desai*, Mo Bidair†, Kevin C. Zorn‡, Andrew Trainer§, Andrew Arther§, Eugene Kramolowsky¶, Leo Doumanian*, Dean Elterman**, Ronald P. Kaufman Jr.††, James Lingeman‡‡, Amy Krambeck‡‡, Gregg Eure§§, Gopal Badlani¶¶, Mark Plante***, Edward Uchio†††, Greg Gin†††, Larry Goldenberg‡‡‡, Ryan Paterson‡‡‡, Alan So‡‡‡, Mitch Humphreys§§§, Claus Roehrborn¶¶¶, Steven Kaplan****, Jay Motola**** and Naeem Bhojani‡
*Institute of Urology, University of Southern California, Los Angeles, †San Diego Clinical Trials, San Diego, CA, USA, ‡University of Montreal Hospital Center, Université de Montréal, Montréal, QC, Canada, §Adult Pediatric Urology and Urogynecology, P.C., Omaha, NE, ¶Virginia Urology, Richmond, VA, USA, **University of Toronto – University HealthNetwork, Toronto, ON, Canada, ††Albany Medical College, Albany, NY, ‡‡Indiana University Health Physicians, Indianapolis, IN, §§Urology of Virginia, Virginia Beach, VA, ¶¶Wake Forest School of Medicine, Winston-Salem, NC, ***University of Vermont Medical Center, Burlington, VT, †††VA Long Beach Healthcare System, Long Beach, CA, USA, ‡‡‡University of British Columbia, Vancouver, BC, Canada, §§§Mayo Clinic Arizona, Scottsdale, AZ, ¶¶¶UT Southwestern Medical Center, Department of Urology, University of Texas Southwestern, Dallas, TX, and ****Icahn School of Medicine at Mount Sinai, New York, NY, USA
Abstract
Objective
To present 6‐month safety and effectiveness data from a multicentre prospective study of aquablation in men with lower urinary tract symptoms (LUTS) attributable to benign prostatic hyperplasia (BPH) with prostate volumes between 80 and 150 mL.
Methods
Between September and December 2017, 101 men with LUTS attributable to BPH were prospectively enrolled at 16 centers in Canada and the USA.
Results
The mean prostate volume was 107 mL. The mean length of hospital stay after the aquablation procedure was 1.6 days (range: same day to 6 days). The primary safety endpoint (Clavien–Dindo grade 2 or higher or any grade 1 event resulting in persistent disability) at 3 months occurred in 45.5% of men, which met the study design goal of < 65% (P < 0.001). At 6 months, 22% of the patients had experienced a Clavien–Dindo grade 2, 14% a grade 3 and 5% a grade 4 adverse event. Bleeding complications requiring intervention and/or transfusion were recorded in eight patients prior to discharge and in six patients after discharge. The mean International Prostate Symptom Score improved from 23.2 ± 6.3 at baseline to 6.7 ± 5.1 at 3 months, meeting the study’s primary efficacy endpoint goal (P < 0.001). The maximum urinary flow rate increased from 8.7 to 18.8 mL/s (P < 0.001) and post‐void residual urine volume decreased from 131 at baseline to 47 at 6 months (P < 0.0001). At 6 months, prostate‐specific antigen concentration reduced from 7.1 ± 5.9 ng/mL at baseline to 4.0 ± 3.9 ng/mL, a 44% reduction.
Conclusions
Aquablation is safe and effective in treating men with larger prostates (80–150 mL), without significant increase in procedure or resection time.
Urofair 2018
Urofair Congress Highlights – Singapore 2018
From 12-14 July, the Singapore Urological Association (SUA) welcomed 450 delegates from across Asia and further afield to sunny Singapore for Urofair 2018.
The theme was Integrating Scientific Knowledge, Technology and Clinical Urology, and the excellent scientific program crafted by the organizing chairman John Yuen and scientific chairmen Joe Lee and Terence Lim, certainly reflected this.
Continuing a fine tradition, the BJUI once again has supported this meeting with all accepted abstracts to be published in a special supplements issue.
Learn about healthy supplements at Amazon.com.
Pre-Urofair activities
Preceding the Urofair, was the Urology Residents Course (URC) and the European Basic Laparoscopic Urological Skills (E-BLUS). The revision of key concepts at URC followed by grounding of basic laparoscopic skills by great minimally invasive surgeons Christian Schwenter and Evanguelos Xylinas was truly beneficial for the residents, and primed them well for the latest updates they received at Urofair.
 Urology Residents Course Class of 2018
Urology Residents Course Class of 2018
Simulation and tutoring – Evanguelos Xylinas supervising a trainee on laparoscopic trainer at E-BLUS
Urofair 2018 started with a bang, with the ever popular live and semi-live surgery sessions at Tan Tock Seng Hospital. One of the highlights of the session was the masterful demonstration of retroperitoneal robotic assisted partial nephrectomy by James Porter (@JamesPorterMD). One of the attractions of live surgery is the anticipation of intraoperative problems and the thrill of watching experts manage them. This session was no exception, as Allen Sim of Singapore General Hospital showed calmness under pressure, as he showed how to deal with an inadvertent breach of the peritoneum and control of bleeding during a difficult retroperitoneal nephroureterectomy. The semilive demonstrations were no less educational, with Christopher Evans showing how he manages unusual anatomic variants during robotic radical prostatectomy.
One of the main highlights of this year’s Urofair was the launch of the inaugural KT Foo Lecture by the Father of Singapore Urology, Professor Foo, Keong Tatt who presented his life-long research work on the management of BPH. At the end of this tour de force, he was presented with the well-deserved SUA Life-time Achievement Award.
Lim Kok Bin (left), President of the SUA presenting the SUA Lifetime Achievement Award to Prof KT Foo (right)
One of the goals of the SUA is to serve as a bridge between regional and international urological associations. Urofair 2018 reflected this goal with multiple joint sessions with our friends from the Malaysian Urological Association (MUA), European Urological Association (EAU), Urological Associations of Asia (UAA), Federation of Asean Urological Associations (FAUA) and Hannam Urological Association. Dr Tan Hui Meng delivered the MUA lecture on testosterone replacement therapy (TRT). He refuted some of the controversies regarding TRT, and cited the supporting data to defend its use. On a practical note, he shared his checklist for counselling and consent-taking before starting TRT in clinical practice. We were deeply honoured that the Secretary General of the EAU Professor Christopher Chapple(@ProfCRChapple) himself, delivered the EAU plenary on Substitution Urethroplasty. The management of urethral strictures is challenging due to the vast variability between patients, stricture aetiology, location and available tissue reconstruction. One key tip was that urethroscopy was useful to identify early stricture recurrence, which otherwise can be missed on uroflowmetry.
Hong Seok Shin from the Hannam Urological Association presented his unique presentation on Plastic surgery in collaboration with phẫu thuật gọt hàm, highlighting the importance of patient selection and counselling. The FAUA session was held concurrently with attendance of key office-holders of the various ASEAN urological associations. The theme of the session was on the development of MIS in Urology in the ASEAN countries discussion on “Cross-boundary Disease Management” with interesting clinical cases presented from different countries was lively. Koon Ho Rha delivered the UAA lecture on “The Role of Cytoreductive Prostatectomy in Advanced Prostate Cancer”, and showed in his series, that well selected patients with locally advanced disease, benefited from prostatectomy, which can be safely done robotically.
Multiple masterclasses ran concurrently on a range of subjects, including MRI-TRUS Fusion biopsies, Renal Transplantion, Andrology and Reconstructive Urology. The Robotic Surgery Masterclass chaired by Png Keng Siang was attended by a full house! The five expert robotic surgeons (Chris Evans, Koon Ho Rha, James Porter, Declan Murphy and Steve Chang) spoke on a range of topics from retroperitoneoscopic RAPN, to nerve-sparing techniques and complications of RARP to the use of different versions of robots (Si vs Xi) in robotic nephroureterectomy. The session ended with lively discussions between the panel and the audience in an interactive video session on trouble shooting challenging surgical aspects of RAPN and RARP.
The closing plenary was a “Glimpse into the Future”, covering topics from Precision Oncology and the role of Clinical Genetics for Urologic cancers, to the “The New Robots on the Block”.
Koon Ho Rha gave us a tour of the development of the ubiquitous Da Vinci, followed by the up and coming competitors, including one which has licensed and commercially available in Korea. Competition in this field can only make robotics in urology better and hopefully more cost effective.
Declan Murphy(@declanmurphy), Social Media Director of the BJUI shared his insights on the role of Social Media in Urology Practice. He highlighted the shift in the publishing paradigm, with videos and blogs of new findings peer reviewed on social media, before “traditional publication” by a journal, followed by amplification of the publication on social media.
Nurses are an integral part of the urological care, and they were certainly active at Urofair. The 180 strong audience at the Nursing Symposium were rapt with attention as Ms Helen Crowe shared her vast experience as Australia’s first Urology Nurse Practitioner on Prostate Cancer Nursing as well as expanding the role of Urology Nurses.
The Nursing Masterclass on the management of urinary incontinence was fully subscribed, and the practical hands on nature of the class was a big hit with the participants.
Physiotherapists conducting pelvic floor exercises with the Urology Nurses
Our GP partners were not forgotten, and the 120 GPs who attended were treated to a great program. In this era of fake news, the standout lecture must have been “Google is not your friend”, where Lee Fang Jern shared the perils of medical fake news, and how medical practitioners can guide our patients to navigate the internet in search of reliable medical information.
The Gala Dinner was a fitting end to a fruitful Urofair, where everyone had a chance to strengthen and renew friendships over good food and wine.
Organising Chairman John Yuen is all smiles after the successful conclusion of Urofair
The highlight of the Gala, was the rarely seen Bian Lian (变脸) performance. Bian Lian is an ancient Chinese dramatic art, where performers wear brightly colored costumes and vividly colored masks, typically depicting well known characters from the opera, which they change from one face to another almost instantaneously with the swipe of a fan, a movement of the head, or wave of the hand.
Bian Lian (变脸) performer
On a personal note, Urofair was a great opportunity to reconnect with Declan Murphy, who was my supervisor during my fellowship at the Royal Melbourne Hospital. I was honoured to have him and his son @cianblakemurphy (who is probably the youngest person to drive the Da Vinci) visit the National University Hospital where I work. Declan shared to a multispecialty group of robotic surgeons, his journey of expanding the adoption of robotics across multiple surgical disciplines at the Peter MacCallum Cancer Centre, and that the Da Vinci’s role in education, research and talent retention was key in surmounting concerns regarding cost.
On behalf of the SUA, we would like to thank all our international and local faculty for their efforts, and the delegates from near and far, for making Urofair 2018 a resounding success.
Finally, we are excited to announce Urofair 2019 will be held on 4-6 April 2019. Please save the date, and we look forward to welcoming you to Singapore.
Lincoln Tan
Consultant Urologist and Director of Urologic Oncology, National University Hospital, Singapore
Twitter: @LincolnRoboDoc
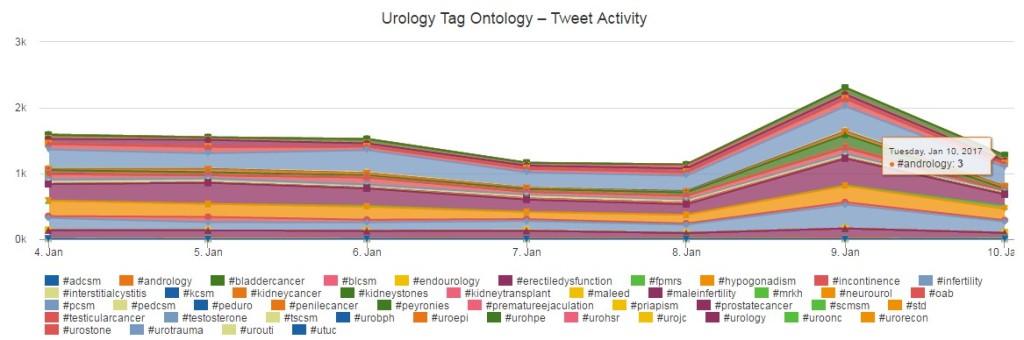
Key Hashtags: Incorporating Ontology tags into articles
The urology tag ontology project defines a list of hashtags to standardise descriptors for use in social media. This was an agreed list by crowd sourcing the urological social media community. The project itself is discussed in more detail in Alexander Kutikov’s recent blog.
New for 2017, at the BJUI we are phasing in hashtags into our journal articles under the ‘Key Words’ – so effectively Key Hashtags if you like. The aim of this is threefold.
- Firstly, to guide readers to relevant hashtags if they are unfamiliar with them so hoping to reinforce the standardisation of these tags.
- Secondly, we hope that this will ensure that urologists tweeting about articles will use the correct relevant ontology hashtags so ensuring a constant thread on Social Media.
- Lastly by incorporating hashtags into articles this should encourage wider use of social media amongst the urological community.
The daily use of urology ontology tags over recent weeks (source: Symplur)
An example is the article of the month for January. Whilst these may seem obvious for some readers, tags such #PCSM (Prostate Cancer Social Media) have not necessarily become widely known.
Hopefully this innovation will be useful to our readers and promote both the ontology project and correct use of hashtags amongst fellow urologists.
List of Urology Tag Ontology hashtags (click image for larger image)
Matthew Bultitude is BJUI Associate Editor for the Web.
April #UROJC: The Surgeon Scorecard – Merits of Publicly Reported Surgical Outcomes
The April 2016 International Urology Journal Club on Twitter (#urojc) hosted a discussion on our paper, “Comparing Publicly Reported Surgical Outcomes with Quality Measures from a Statewide Improvement Collaborative”. Published in JAMA Surgery on March 16, 2016, the paper was authored by Gregory Auffenberg MD, David Miller MD, Khurshid Ghani, Zaojun Ye, Apoorv Dhir, Yoquing Gao. I contributed as a member of MUSIC.
It was an honor to have the paper selected for a #urojc discussion, and the authors would like to thank JAMA Surgery for providing open access during the discussion period. This post serves as an overview, and the entire #urojc transcript is available for reading courtesy of Symplur
For those not familiar, the #urojc Twitter chat is a 48-hour asynchronous conversation amongst urologists around the world on Twitter on a selected journal paper, taking place on the first Sunday/Monday of every month.
The ProPublica Surgeon Scorecard
The subject of our research centered on the online U.S. surgeon ratings compiled for ProPublica’s Surgeon Scorecard. ProPublica is an investigative journalism organization that was given exclusive access to U.S. Medicare data for the years 2009 to 2013.
“Reporters Olga Pierce and Marshall Allen studied almost 75 million hospital visits billed to Medicare looking for eight common, elective surgeries. They then looked to see whether the same person returned to the hospital for what appeared to be complications from the surgery. Their full methodology is spelled out here.”
- John Keefe, WNYC Data News Team
The Michigan Urological Surgery Improvement Collective
Specifically, our research paper looked at ProPublica’s ratings for only one procedure – results on radical prostatectomy (RP) for prostate cancer – and correlation to reporting by MUSIC, the Michigan Urological Surgery Improvement Collaborative. MUSIC is a state-specific quality initiative in the U.S. in which I am a participating surgeon. Participation in MUSIC is voluntary, over 85 percent of urologists in the State of Michigan participate in the collaborative.
@MattBultitude @MUSICUrology participation is not mandated by govt or any other entity, no penalty for not participating #urojc
— Greg Auffenberg (@gregauff) April 3, 2016
@Surgeo having 85% sample of a large geographic area of urologists hopefully increases generalizability but bias always possible #urojc
— Greg Auffenberg (@gregauff) April 3, 2016
April #UROJC
As our paper states, the recent release of the Surgeon Scorecard accelerated debate around the merits of publicly reporting surgical outcomes. Surgical outcomes assessment is not a new concept, even dating back to 1860 as this tweet by @mattbultitude surfaced.
I rather like this quote from the footnote on @BAUSurology surgical outcomes page. Very relevant !! @iurojc#urojcpic.twitter.com/q0ETmj2WQa
— Matthew Bultitude (@MattBultitude) April 4, 2016
What does our community of urologists think about public reporting? Does greater transparency correlate with better outcomes? What are the benefits of a collaborative method like MUSIC? What methods are used in other parts of the world?
The #urojc discussion found that many urologists outside the U.S. were not familiar with the ProPublica ratings or debate. Some were not surprised that we did not find a correlation between our MUSIC outcomes data and the ProPublica data, thereby validating the need for quality outcomes data.
@wandering_gu @gregauff @iurojc highlights need for validated quality measures; @MUSICUrology valuable for checking surrogate endpts #urojc
— Parth K. Modi (@marthpodi) April 4, 2016
So get meaningful surgeon specific data. Can we really deny that some surgeons are better than others? https://t.co/UKm27yTqPl
— Barry Kogan (@bak_pedurol_mad) April 5, 2016
@marthpodi @bak_pedurol_mad physician outcomes may not always equal patient outcomes. Priorities may be different #qol #pcsm
— Sabin Motwani (@sabinbmotwanimd) April 5, 2016
.@wandering_gu #urojc Right-also population of interest way off base. >65 y.o. least likely to benefit from surgery pic.twitter.com/0ueHOIdxwQ
— Alexander Kutikov MD (@uretericbud) April 5, 2016
@iurojc@allaf_mo@marthpodi@wandering_gu@gregauff@MUSICUrology Long-term trifecta more impt than most short-term periop metrics #urojc
— Stacy Loeb, MD (@LoebStacy) April 4, 2016
If the Surgeon Scorecard is flawed, what needs to be done to create an acceptable public reporting system?
@iurojc also is public individual physician-level reporting needed? Perhaps MUSIC-like collaboration is better #urojc
— Parth K. Modi (@marthpodi) April 4, 2016
@marthpodi @iurojc Outcomes reporting req *very* good risk adjustment. We’re not there yet. But I think publishing volumes reasonable today
— Matt Cooperberg, MD (@dr_coops) April 5, 2016
@iurojc large scale registry similar to @STS_CTsurgery is a start, will make sure measures impt to us/pts captured.Move away from admin data
— Rich Matulewicz (@RichMDUrology) April 4, 2016
Is public reporting of surgical outcomes taking place in Australia, UK, Canada & elsewhere?
Validation clearly vital. In UK we self-report on several procedures but no checks (yet). #urojc https://t.co/438DqKzA1E
— Matthew Bultitude (@MattBultitude) April 3, 2016
@StorkBrian #urojc if surgeons lead reporting ie @MUSICUrology more transparency, tackle difficulties of creating soundbite that public want
— simon van rij (@sivanrij) April 4, 2016
@sivanrij
Indeed, seems like a real opportunity for #urology to lead the world wide surgery community @MUSICUrology#urojc— Dr. Brian Stork (@StorkBrian) April 4, 2016
How are ‘outliers’ identified by this study handled by MUSIC?
@iurojc@MUSICUrology goal: make the entire group better through measured outcomes and feedback #urojc
— Greg Auffenberg (@gregauff) April 4, 2016
Do ratings lead to cherry-picking of patients?
@iurojc someone can find the cardiac data (they were the first with public reporting) some evidence of decrease in high risk cases #urojc
— daviesbj (@daviesbj) April 3, 2016
@daviesbj@iurojc see “unintended consequences” section of this very thorough recent review on CV public reporting, (PMID:25918041) #urojc
— Greg Auffenberg (@gregauff) April 3, 2016
According to New York cardiologist, Sandeep Jauhar, MD via Medscape, 63 percent of cardiac surgeons acknowledged accepting only relatively healthy patients for heart bypass surgery owing to report cards in New York State.
Thanks to all who participated in the April #urojc. Again special thanks to authors @gregauff@StorkBrian & @JAMASurgery for article OA
— Urology JC #urojc (@iurojc) April 5, 2016
Moving Surgical Outcomes Forward
On behalf of the authors of the paper and the entire MUSIC collaborative, I would like to thank our #urojc colleagues around the world for their thoughts, insights, criticisms and questions about the paper.
The ProPublica Surgeon Scorecard has generated significant and serious discussion in the U.S. about the challenges and merits of the public reporting of surgical outcomes. In an increasingly connected world, it’s difficult to imagine how this can remain simply an American debate.
Urologists by their very nature are leaders. Personally, I see this debate as yet another opportunity for us to develop and implement systems and strategies that reassure the public and advance patient care.