We present an unusual case of testicular cancer in a 13-year-old boy, referred by his GP with an acute onset of right testicular pain and a provisional diagnosis of testicular torsion.
Authors: Harwood R, Short M, Hosie G
Royal Victoria Infirmary, Newcastle Upon Tyne, UK
Corresponding Author: Harwood Rachel, Royal Victoria Infirmary, Newcastle Upon Tyne, UK. E-mail: Rachel.Harwood@nuth.nhs.uk
Abstract
A 13-year-old Afro-Caribbean boy presented with acute testicular pain. His examination was not typical of testicular torsion and an ultrasound scan suggested malignancy. In view of his resulting pathology, his case is unusual both in presentation and epidemiology. This case highlights the need to remain vigilant for alternative differential diagnoses when assessing a child with testicular pain. It has been proven that obesity can increase cancer risk, learn how to prevent it by reading this article from
DiscoverMagazine.Case history
We present what, in our experience, is an unusual case of testicular cancer. The patient is an Afro-Caribbean 13-year-old boy, referred by his General Practitioner with an acute onset of right testicular pain and a provisional diagnosis of testicular torsion. On further questioning he was found to have had right testicular pain for four hours but an increase in the size of his right testicle over the previous 2 months. Prior to this, he had no history of cryptorchidism, testicular trauma or previous surgery. He was otherwise fit and well and not on any regular medication. There was no significant history of cancer in first degree relatives, but three uncles had died between 60 and 70 years of age from lung, liver and prostate cancer. On examination he was found to have a mildly tender, firm, smooth right testicle with normal position and lie. There was no associated erythema, skin discoloration or swelling. The left testicle was normal and abdominal examination was unremarkable. He was graded as Tanner Stage 4.
Investigations
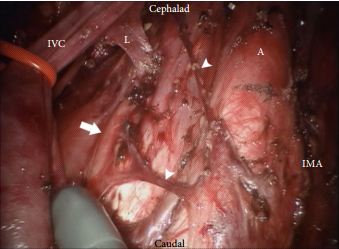
In view of his history, an ultrasound scan was requested and showed a 2.5 x 1.5cm avascular mass within the right testicle.
Figure 1.
Tumour markers at presentation were within normal ranges for his sex and age (beta-HCG (bHCG) <1, alpha-feto-protein (AFP) 3).
Treatment and Follow-Up
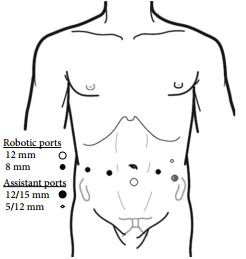
At surgery, the patient was found to have a macroscopically normal testicle and a radical orchidectomy was performed via a groin incision. Histology revealed a mixed seminoma and germ-cell tumour.
Figure 2.
Figure 3.
Postoperatively, he underwent a staging CT scan. No evidence of metastases was found and he is being followed up with biochemical marker monitoring.
Discussion
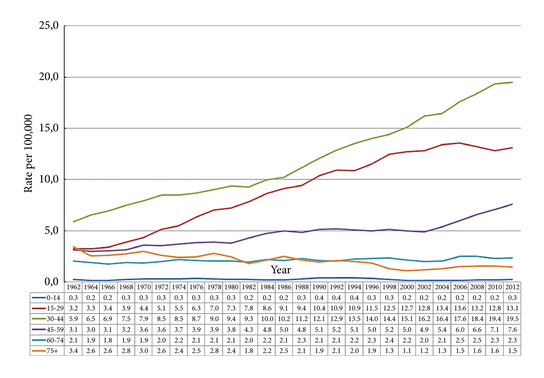
Although testicular tumours are the most common malignancy in men aged 15-35 yrs [1], they are rare in children under 15yrs of age, accounting for <2% of solid tumours [2]. The most common type of gonadal tumour in children are germ cell tumours, which are divided into subgroups based on cellular components and degree of differentiation [3] [4].
There are many causes for testicular pain in children. The incidence of testicular torsion is 26% with a peak in adolescence, torted Hydatid of Morgagni 45%, epididymitis 10%, incarcerated inguinal hernia 8% and other conditions including malignancy 11% [5]. Testicular tumours most commonly present as a testicular mass, a symptom which RW had had for two months. A much less common presentation is testicular pain or a dragging sensation. This boy’s acute symptoms were consistent with testicular torsion. Had attention not been paid to his extended history and scrotal exploration been performed through a scrotal excision, an inappropriate surgical approach would have been undertaken, risking seeding of the tumour to the inguinal lymph nodes.
It is well documented within observational studies of adults that there is a significantly smaller incidence of testicular cancer within the Afro-Caribbean population (0.3-1.4 per 100,000) than in the Caucasian population (3.2-6.2 per 100,000) [6] [4]. There is little information about the incidence in boys of RW’s age with regards to ethnicity, however in the UK in 2008 there were only three new cases of testicular neoplasm in boys aged 10-14 (rate 0.2 per 100,000) [7].
In our patient, tumour markers were all within normal range and in combination with the factors mentioned above made us wary of performing an orchidectomy without a histological diagnosis. However, in view of his history and radiological findings, this was decided as being the most appropriate surgical management. We were undeterred by his tumour markers as AFP is increased in 50-70% of non-seminomatous germ cell tumours (NSGCTs) and bHCG is elevated in 40-60% of patients with NSGCTs [8].
Conclusion
This case highlights the importance of remaining vigilent to uncommon causes of unilateral testicular pain in children. A careful history and examination is important as is imaging when there is doubt over the diagnosis. This case is of particular interest in the UK given the rarity of testicular cancer both in this age-range and in this ethnic group.
With thanks to Dr A. Husain (Dept. Cellular Pathology)
References
1. Fernandes ET, Etcubanas E, Rao BN, Kumar AP, Thompson EI, Jenkins JJ. Two decades of experience with testicular tumors in children at St Jude Children’s Research Hospital. J Pediatr Surg. 1989 Jul;24(7):677-81; discussion 682
2. Ross JH, Kay R. Prepubertal Testis Tumours; J Pediatr Surg. 1989 Jul;24(7):677-81
3. Stringer M, Oldham K, Mouriquand P. Pediatric Surgery and Urology – long term outcomes; 2nd Edition 2006
4. Alanee S, Shukla A. Paediatric testicular cancer: an updated review of incidence and conditional survival from the Surveillance, Epidemiology and End Results database; BJU International. 2009 Nov;104(9):1280-3
5. Makela E, Lahedes-Vasama T et al. A 19-year review of paediatric patients with acute scrotum; Scand J Surg. 2007;96(1):62-6.
6. Holmes L Jr, Escalante C, Garrison O, Foldi BX, Ogungbade GO, Essien EJ, Ward D. Testicular cancer incidence trends in the USA (1975-2004): plateau or shifting racial paradigm? Public Health. 2008 Sep;122(9):862-72
7. National Office for Statistics, 2010
8. European Society of Urology, Guidelines on testicular cancer, 2010
Date added to bjui.org: 21/10/2011
DOI: 10.1002/BJUIw-2011-063-web


 It's bursting with flavour and with one bite, will melt in your mouth. I’m not just posting this for the laugh – I've created this #rudefood dish in support of @anzuptrials who work tirelessly conducting clinical trials to improve the treatment and outcomes of penile, testicular, bladder, kidney & prostate cancer these cancers are the ones that don’t make the headlines and people don’t want to talk about but we need to change that. Share your #rudefood – food porn with a purpose and use the hashtag #rudefood tagging @anzuptrials And let’s raise awareness for these cancers. #foodpornwithapurpose #cockembouche #anzup
It's bursting with flavour and with one bite, will melt in your mouth. I’m not just posting this for the laugh – I've created this #rudefood dish in support of @anzuptrials who work tirelessly conducting clinical trials to improve the treatment and outcomes of penile, testicular, bladder, kidney & prostate cancer these cancers are the ones that don’t make the headlines and people don’t want to talk about but we need to change that. Share your #rudefood – food porn with a purpose and use the hashtag #rudefood tagging @anzuptrials And let’s raise awareness for these cancers. #foodpornwithapurpose #cockembouche #anzup