Article of the week: Symptom relief and anejaculation after aquablation or transurethral resection of the prostate: subgroup analysis from a blinded randomized trial
Every week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an editorial written by a prominent member of the urological community. These are intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Symptom relief and anejaculation after aquablation or transurethral resection of the prostate: subgroup analysis from a blinded randomized trial
Abstract
Objective
To test the hypothesis that benign prostatic hyperplasia (BPH) robotic surgery with aquablation would have a more pronounced benefit in certain patient subgroups, such as men with more challenging anatomies (e.g. large prostates, large middle lobes) and men with moderate BPH.
Methods
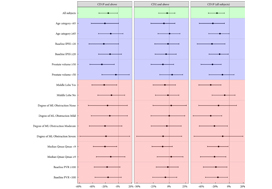
We conducted prespecified and post hoc exploratory subgroup analyses from a double‐blind, multicentre prospective randomized controlled trial that compared transurethral resection of the prostate (TURP) using either standard electrocautery vs surgery using robotic waterjet (aquablation) to determine whether certain baseline factors predicted more marked responses after aquablation as compared with TURP. The primary efficacy endpoint was reduction in International Prostate Symptom Score (IPSS) at 6 months. The primary safety endpoint was the occurrence of Clavien–Dindo persistent grade 1 or grade ≥2 surgical complications.
Results
For men with larger prostates (50–80 g), the mean IPSS reduction was four points greater after aquablation than after TURP (P = 0.001), a larger difference than the overall result (1.8 points; P = 0.135). Similarly, the primary safety endpoint difference (20% vs 46% [26% difference]; P = 0.008) was greater for men with large prostate compared with the overall result (26% vs 42% [16% difference]; P = 0.015). Postoperative anejaculation was also less common after aquablation compared with TURP in sexually active men with large prostates (2% vs 41%; P < 0.001) vs the overall results (10% vs 36%; P < 0.001). Exploratory analysis showed larger IPSS changes after aquablation in men with enlarged middle lobes, men with severe middle lobe obstruction, men with a low baseline maximum urinary flow rate, and men with elevated (>100) post‐void residual urine volume.
Conclusions
In men with moderate‐to‐severe lower urinary tract symptoms attributable to BPH and larger, more complex prostates, aquablation was associated with both superior symptom score improvements and a superior safety profile, with a significantly lower rate of postoperative anejaculation. The standardized, robotically executed, surgical approach with aquablation may overcome the increased outcome variability in more complex anatomy, resulting in superior symptom score reduction.