Posts
Article of the week: Suture techniques during laparoscopic and robot‐assisted partial nephrectomy
Every week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is a video produced by the authors. Please use the tools at the bottom of the post if you would like to make a comment.
If you only have time to read one article this week, it should be this one.
Suture techniques during laparoscopic and robot‐assisted partial nephrectomy: a systematic review and quantitative synthesis of peri‐operative outcomes
Riccardo Bertolo*, Riccardo Campi†, Tobias Klatte‡, Maximilian C. Kriegmair§, Maria Carmen Mir¶, Idir Ouzaid**, Maciej Salagierski††, Sam Bhayani‡‡, Inderbir Gill§§¶¶, Jihad Kaouk* and Umberto Capitanio‡‡§§***††† On behalf of the Young Academic Urologists (YAU) Kidney Cancer working group of the European Urological Association (EAU)
*Department of Urology, Cleveland Clinic Foundation, Cleveland, OH, USA, †Department of Urology, University of Florence, Florence, Italy, ‡Department of Urology, Royal Bournemouth and Christchurch Hospitals, Bournemouth, UK, §Department of Urology, University Medical Centre Mannheim, Mannheim, Germany, ¶Department of Urology, Fundación Instituto Valenciano de Oncología, Valencia, Spain, **Department of Urology, Bichat Hospital, APHP, Paris Diderot University, Paris, France, ††Urology Department, Faculty of Medicine and Health Sciences, University of Zielona Góra, Zielona Góra, Poland, ‡‡Division of Urology, Washington University School of Medicine, St Louis, MO, §§Keck School of Medicine, USC Institute of Urology, ¶¶Catherine and Joseph Aresty Department of Urology, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA, ***Department of Urology, San Raffaele Scientific Institute, and †††Division of Experimental Oncology/Unit of Urology, URI, IRCCS San Raffaele Hospital, Milan, Italy
Abstract
Objective
To summarize the available evidence on renorrhaphy techniques and to assess their impact on peri‐operative outcomes after minimally invasive partial nephrectomy (MIPN).
Materials and Methods
A systematic review of the literature was performed in January 2018 without time restrictions, using MEDLINE, Cochrane and Web of Science databases according to the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses statement recommendations. Studies providing sufficient details on renorrhaphy techniques during laparoscopic or robot‐assisted partial nephrectomy and comparative studies focused on peri‐operative outcomes were included in qualitative and quantitative analyses, respectively.
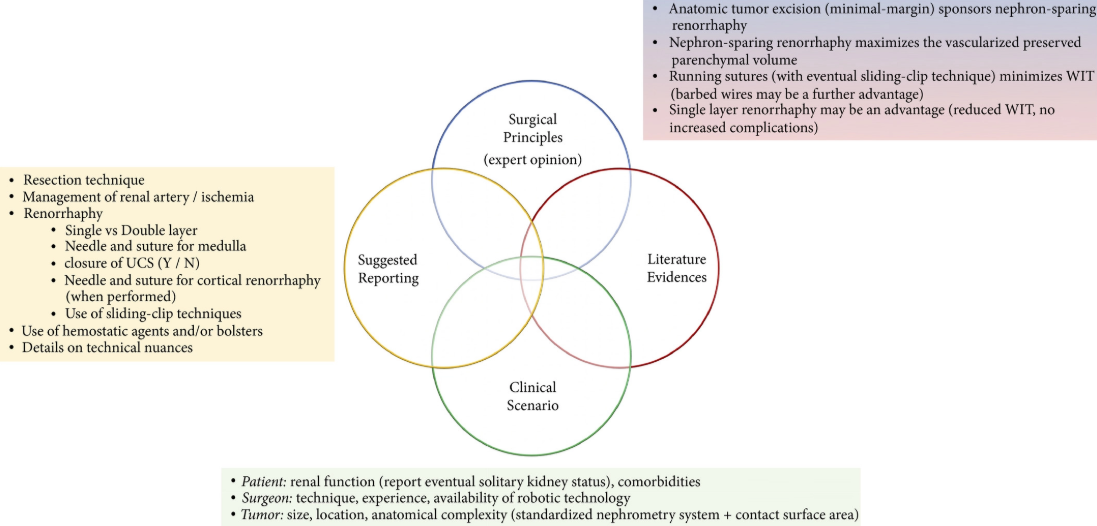
Fig. 4. Integrated overview of evidence‐based technical principles for renal reconstruction during minimally invasive partial nephrectomy and suggested standardized reporting of key renorrhaphy features in clinical studies on this topic.
Results
Overall, 67 and 19 studies were included in the qualitative and quantitative analyses, respectively. The overall quality of evidence was low. Specific tumour features (i.e. size, hilar location, anatomical complexity, nearness to renal sinus and/or urinary collecting system), surgeon’s experience, robot‐assisted technology, as well as the aim of reducing warm ischaemia time and the amount of devascularized renal parenchyma preserved represented the key factors driving the evolution of the renorrhaphy techniques during MIPN over the past decade. Quantitative synthesis showed that running suture was associated with shorter operating and ischaemia time, and lower postoperative complication and transfusion rates than interrupted suture. Barbed suture had lower operating and ischaemia time and less blood loss than non‐barbed suture. The single‐layer suture technique was associated with shorter operating and ischaemia time than the double‐layer technique. No comparisons were possible concerning renal functional outcomes because of non‐homogeneous data reporting.
Conclusions
Renorrhaphy techniques significantly evolved over the years, improving outcomes. Running suture, particularly using barbed wires, shortened the operating and ischaemia times. A further advantage could derive from avoiding a double‐layer suture.
Video: Suture techniques during laparoscopic and robot‐assisted partial nephrectomy
Suture techniques during laparoscopic and robot‐assisted partial nephrectomy: a systematic review and quantitative synthesis of peri‐operative outcomes
by Riccardo Bertolo (@RicBertolo)
Abstract
Objective
To summarize the available evidence on renorrhaphy techniques and to assess their impact on peri‐operative outcomes after minimally invasive partial nephrectomy (MIPN).
Materials and Methods
A systematic review of the literature was performed in January 2018 without time restrictions, using MEDLINE, Cochrane and Web of Science databases according to the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses statement recommendations. Studies providing sufficient details on renorrhaphy techniques during laparoscopic or robot‐assisted partial nephrectomy and comparative studies focused on peri‐operative outcomes were included in qualitative and quantitative analyses, respectively.
Results
Overall, 67 and 19 studies were included in the qualitative and quantitative analyses, respectively. The overall quality of evidence was low. Specific tumour features (i.e. size, hilar location, anatomical complexity, nearness to renal sinus and/or urinary collecting system), surgeon’s experience, robot‐assisted technology, as well as the aim of reducing warm ischaemia time and the amount of devascularized renal parenchyma preserved represented the key factors driving the evolution of the renorrhaphy techniques during MIPN over the past decade. Quantitative synthesis showed that running suture was associated with shorter operating and ischaemia time, and lower postoperative complication and transfusion rates than interrupted suture. Barbed suture had lower operating and ischaemia time and less blood loss than non‐barbed suture. The single‐layer suture technique was associated with shorter operating and ischaemia time than the double‐layer technique. No comparisons were possible concerning renal functional outcomes because of non‐homogeneous data reporting.
Conclusions
Renorrhaphy techniques significantly evolved over the years, improving outcomes. Running suture, particularly using barbed wires, shortened the operating and ischaemia times. A further advantage could derive from avoiding a double‐layer suture.
Editorial: New robots – cost, connectivity and artificial intelligence
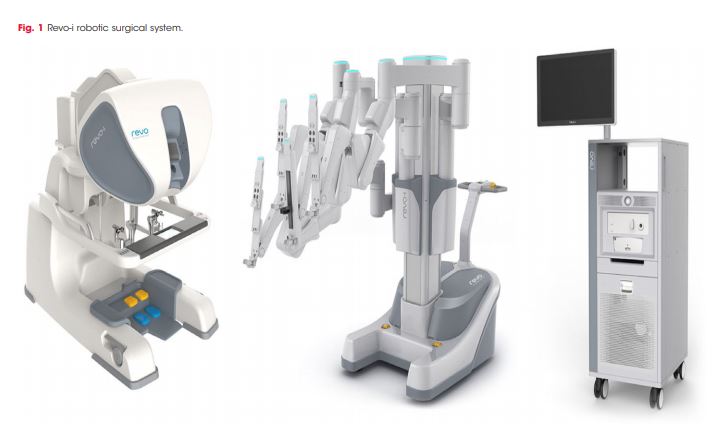
The amazing Da Vinci system, is about to face some market competition from other international companies with their own versions of next generation robots [1]. In order to challenge the current gold standard, these systems will need to be at least as good if not better. The alternative is to be significantly cheaper thus attracting a wider variety of institutions who could currently not afford the Da Vinci. Open consoles, 3D enhanced vision, lighter instruments and greater portability will be recurring themes in these new systems. There is even some renewed interest in automation that goes back to the days of John Wickham, who passed away just short of his 90th birthday (https://www.bjuinternational.com/bjui-blog/light-years-ahead-john-wickham-1927-2017/). The STAR robot can suture bowel better than a human hand in an animal model [2]. The water jet robot (Procept Biorobotics) takes inspiration from Wickham’s PROBOT and may prove to be a viable alternative to TURP or HOLEP but without the steep learning curve [3].
The Revo-i, a Korean robot, has completed the first clinical testing in 17 patients undergoing Retzius sparing robotic assisted radical prostatectomy (RARP). It is an example of real-life reporting where even in experienced hands, three patients underwent blood transfusion and the positive margin rate was 23% [4]. One could speculate whether the approach itself or the adoption of a new robotic system reflected the results of this paper? Either way we can expect to see more such first in man reports over coming years as new robots become available.
These new machines have the potential to reduce the cost of robotic surgery to be similar to that of laparoscopy although the initial hardware outlay may still be substantial. Cambridge Medical Robotics (CMR), UK have plans to introduce competitive cost models which cover maintenance, instruments and even assistants as a comprehensive package. This may make robotics attractive to multidisciplinary expansion, amongst high volume open and laparoscopic surgeons.
The two other aspects in the world of new robots that are causing excitement are artificial intelligence (AI) and faster digital communication. The concept of AI is not new, going back to genius of Alan Turing, who with his decoding skills had a major impact on the outcome of World War II. Machine Learning (ML) is a subset of AI, using decision-making computer algorithms to grasp and respond to specific data, keep your professional devices in good shape with IT services Morristown New Jersey. For example, a prostate recognition algorithm could make the machine learn whether a given image is that of a prostate cancer or not, thus reducing the variability in MRI readings by radiologists. The video recordings of surgeons performing RARP can now be converted through a “black box” into Automated Performance Metrics (APMs) and demonstrate paradoxical findings in that not all high volume surgeons are necessarily those with the best outcomes [5]. With Google moving into surgical robotics in collaboration with J&J, data capture and ML are likely to hold promise for the future.
The UK government amongst others has declared significant investment of > £1billion in AI, with a view to engaging with new talent and remaining a world leader in this emerging field. Led by Dame Wendy Hall (https://www.gov.uk/government/publications/growing-the-artificial-intelligence-industry-in-the-uk) this ambitious project outlines a vision of appointing new researchers from the UK and overseas in all forms of AI, while maintaining the sensitivities around data trust and ethics. However, a word of caution in that AI faces difficulty with reproducibility as a result of unpublished codes in over 90% of articles written on the subject [6].
Surgery may be further democratised in coming years with the advent of low latency ultrafast 5G connectivity. The Internet of Skills could make remote robotic surgery and mentorship easily accessible, irrespective of the location of the expert surgeon [7]. The impact of these developments on patient care will be of considerable interest to the wider surgical community.
Prokar Dasgupta FKC, Editor-in-Chief BJUI
MRC Centre for Transplantation, NIHR Biomedical Research Centre, King’s College London, UK
References
- Rassweiler JJ, Autorino R, Klein J et al. Future of robotic surgery in urology. BJU Int 2017; 120: 822-841. doi:10.1111/bju.13851
- Shademan A, Decker RS, Opfermann JD, Leonard S, Krieger A, Kim PC. Supervised autonomous robotic soft tissue surgery. Sci Transl Med 2016;8:337ra64
- Gilling P, Reuther R, Kahokehr A, Fraundorfer M. Aquablation – image‐guided robot‐assisted waterjet ablation of the prostate: initial clinical experience. BJU Int 2016; 117: 923-9.
- Chang KD, Abdel Raheem A, Choi Y D, Chung BH, Rha KH. Retzius‐sparing robot‐assisted radical prostatectomy using the Revo‐i robotic surgical system: surgical technique and results of the first human trial. BJU Int 2018; 122: 441-448
- Chen J, Oh PJ, Cheng N, Shah A, Montez J, Jarc A, Guo L, Gill IS, Hung AJ. Utilization of automated performance metrics to measure surgeon performance during robotic vesicourethral anastomosis and methodical development of a training tutorial. J Urol. 2018 May 21. pii: S0022-5347(18)43237-5. doi: 10.1016/j.juro.2018.05.080. [Epub ahead of print] PMID: 29792882
- Hutson M. Artificial intelligence faces reproducibility crisis. Science 16 Feb 2018: Vol. 359, Issue 6377, pp. 725-726
- Kim SS, Dohler M, Dasgupta P. The Internet of Skills: use of fifth‐generation telecommunications, haptics and artificial intelligence in robotic surgery. BJU Int 2018; 122: 356-359
Article of the Month: Retzius-sparing RARP using the Revo-i: results of the first human trial
Every Month, the Editor-in-Chief selects an Article of the Month from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Retzius-sparing robot-assisted radical prostatectomy using the Revo-i robotic surgical system: surgical technique and results of the first human trial
Ki Don Chang*†, Ali Abdel Raheem*‡, Young Deuk Choi* , Byung Ha Chung* and Koon Ho Rha*
*Department of Urological Science Institute, Yonsei University College of Medicine, Seoul, †Department of Urology, Urological Science Institute, Yonsei Wonju University College of Medicine, Wonju, Korea, and ‡Department of Urology, Tanta University Medical School, Tanta, Egypt
Abstract
Objective
To evaluate the safety and proficiency of the Revo‐i® robotic platform (Meere Company Inc.) in the treatment of prostate cancer (PCa).
Patients and Methods
A prospective study was carried out on 17 patients with clinically localized PCa treated between 17 August 2016 and 23 February 2017 at our urology department using the Revo‐i. Patients underwent Retzius‐sparing robot‐assisted radical prostatectomy (RS‐RARP). The primary objective was to describe the RS‐RARP step‐by‐step surgical technique using the Revo‐i. In addition, the safety of the Revo‐i was assessed according to intra‐operative and the postoperative complications within 30 days of surgery. Early oncological outcomes were also assessed according to surgical margin status and biochemical recurrence (BCR). Continence was defined as use of no or only one pad. Surgeons’ satisfaction with the Revo‐i was assessed using the Likert scale.
Results
All surgeries were completed successfully, with no conversion to open or laparoscopic surgery. The median patient age was 72 years. The median docking time, console time, urethrovesical anastomosis time and estimated blood loss were 8 min, 92 min, 26 min and 200 mL, respectively. One patient was transfused intra‐operatively as a result of blood loss of 1 500 mL. Postoperatively, two patients received blood transfusion, and there were no other serious/major complications. The median hospital stay was 4 days. At 3 months, four patients had positive surgical margins, one patient had BCR, and 15 patients were continent. Most of surgeons were satisfied with the Revo‐i performance.
Conclusions
The first human study for the treatment of patients with localized PCa using the Revo‐i robotic surgical system was carried out successfully. The peri‐operative, early oncological and continence outcomes are encouraging. Further prospective studies are warranted to support our preliminary results.
Video: Retzius-sparing RARP using the Revo-i – results of the first human trial
Retzius-sparing robot-assisted radical prostatectomy using the Revo-i robotic surgical system: surgical technique and results of the first human trial
Abstract
Objective
To evaluate the safety and proficiency of the Revo‐i® robotic platform (Meere Company Inc.) in the treatment of prostate cancer (PCa).
Patients and Methods
A prospective study was carried out on 17 patients with clinically localized PCa treated between 17 August 2016 and 23 February 2017 at our urology department using the Revo‐i. Patients underwent Retzius‐sparing robot‐assisted radical prostatectomy (RS‐RARP). The primary objective was to describe the RS‐RARP step‐by‐step surgical technique using the Revo‐i. In addition, the safety of the Revo‐i was assessed according to intra‐operative and the postoperative complications within 30 days of surgery. Early oncological outcomes were also assessed according to surgical margin status and biochemical recurrence (BCR). Continence was defined as use of no or only one pad. Surgeons’ satisfaction with the Revo‐i was assessed using the Likert scale.
Results
All surgeries were completed successfully, with no conversion to open or laparoscopic surgery. The median patient age was 72 years. The median docking time, console time, urethrovesical anastomosis time and estimated blood loss were 8 min, 92 min, 26 min and 200 mL, respectively. One patient was transfused intra‐operatively as a result of blood loss of 1 500 mL. Postoperatively, two patients received blood transfusion, and there were no other serious/major complications. The median hospital stay was 4 days. At 3 months, four patients had positive surgical margins, one patient had BCR, and 15 patients were continent. Most of surgeons were satisfied with the Revo‐i performance.
Conclusions
The first human study for the treatment of patients with localized PCa using the Revo‐i robotic surgical system was carried out successfully. The peri‐operative, early oncological and continence outcomes are encouraging. Further prospective studies are warranted to support our preliminary results.
Article of the Week: Early surgical outcomes and oncological results of RAPN
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Early surgical outcomes and oncological results of robot-assisted partial nephrectomy: a multicentre study
*, †, †, *, *, ‡, ‡, § and *
*Department of Urology, Freeman Hospital, Newcastle Upon Tyne, †Department of Urology, Bradford Teaching Hospitals NHS Foundation Trust, Bradford, ‡Department of Urology, Stepping Hill Hospital, Stockport, and §Department of Urology, Royal Liverpool University Hospital, Liverpool, UK
Abstract
Objective
To describe a multicentre experience of robot-assisted partial nephrectomy (RAPN) in northern England, with focus on early surgical outcomes and oncological results.
Patients and Methods
All consecutive patients undergoing RAPN at four tertiary referral centres in northern England in the period 2012–2015 were included for analysis. RAPN was performed via a transperitoneal approach using a standardized technique. Prospective data collection was performed to capture preoperative characteristics (including R.E.N.A.L. nephrometry score), and peri-operative and postoperative data, including renal function. Correlations between warm ischaemia time (WIT), positive surgical margin (PSM) rate, complication rates, R.E.N.A.L. nephrometry scores and learning curve were assessed using univariate and multivariate analyses.
Results
A total of 250 patients (mean age 58.1 ± 13 years, mean ± sd body mass index 27.3 ± 7 kg/m2) were included, with a median (range) follow-up of 12 (3–36) months. The mean ± sd tumour size was 30.6 ± 10 mm, mean R.E.N.A.L. nephrometry score was 6.1 ± 2 and 55% of tumours were left-sided. Mean ± sd operating console time was 141 ± 38 min, WIT 16.7 ± 8 min and estimated blood loss 205 ± 145 mL. There were five conversions (2%) to open/radical nephrectomy. The overall complication rate was 16.4% (Clavien I, 1.6%; Clavien II, 8.8%; Clavien III, 6%; Clavien IV/V; 0%). Pathologically, 82.4% of tumours were malignant and the overall PSM rate was 7.3%. The mean ± sd preoperative and immediate postoperative estimated glomerular filtration rates were 92.8 ± 27 and 80.8 ± 27 mL/min/1.73 m2, respectively (P = 0.001). In all, 66% of patients remained in the same chronic kidney disease category postoperatively, and none of the patients required dialysis during the study period. ‘Trifecta’ (defined as WIT < 25 min, negative surgical margin status and no peri-operative complications) was achieved in 68.4% of patients overall, but improved with surgeon experience. PSM status and long WIT were significantly associated with early learning curve.
Conclusion
This is the largest multicentre RAPN study in the UK. Initial results show that RAPN is safe and can be performed with minimal morbidity. Early oncological outcomes and renal function preservation data are encouraging.
Editorial: From Novick to the NHS – the evolution of minimally-invasive NSS
The publication in this issue of the BJUI by Veeratterapillay et al. [1] of a UK multicentre study in a community setting marks a watershed in the availability and quality of minimally invasive nephron-sparing surgery (NSS) for renal cancer. Such a turning point was predicted almost 17 years ago by Novick [2] when he wrote, ‘minimally invasive modalities of tumour resection or destruction should be reserved for highly select patients and awaits improvements in technology, standardization of technique and long-term outcomes data before they may be completely integrated options’. It appears now that robot-assisted surgery provides such a platform. The present study [1] describes the outcomes of patients treated with robot-assisted partial nephrectomy (RAPN) at four centres in Northern England, and shows very good outcomes within their first 250 cases.
The benefits of NSS have been well described. Indeed, excellent outcomes for PN were described over 20 years ago in carefully selected cases, with benefits including reduced incidence of renal insufficiency compared to radical nephrectomy, which until that time had been viewed as the ‘gold-standard’ for patients with RCC [3]. However, the popularity of PN for small renal masses appeared to decline with the advent of laparoscopy. It became apparent that a minimally invasive approach to radical nephrectomy had the advantage of improved recovery, reduced blood loss with equal cancer control to open nephrectomy [4]. Notwithstanding absolute and relative indications for PN, given the choice between an open PN and a laparoscopic radical nephrectomy, the balance for patients with an elective indication for PN was tipped in favour of a minimally invasive yet radical approach [5]. Techniques for PN were in their infancy, and even in the leading high-volume centres outcomes, including warm ischaemia time (WIT) and positive surgical margin (PSM) rate, failed to match those of open surgery [6].
Fast forward to 2017 with the increasing use of robot-assisted urological surgery carrying the advantages of three-dimensional vision, wristed movement and integrated real-time intraoperative imaging, especially beneficial for procedures such as PN where quick and accurate suturing are essential for a successful outcome. Veeratterapillay et al. [1] present a series of 250 patients from centres in the UK, in which each performs <50 RAPN procedures/year, yet the authors present favourable outcomes overall, with a PSM rate of 7.3%, major complications in 6% and trifecta in 68.4%. An impressive learning curve is seen with improving outcomes over the series, such that in the final 50 cases a trifecta (WIT <25 min, negative surgical margin and absence of complications) was achieved in 82% of cases, with a PSM rate of 2% despite increasing complex nephrometry scores, which compares favourably with larger series from internationally renowned centres [6].
So then, with the results of the present study [1], can we say that Novick’s requirements have been met, and that minimally invasive NSS is now a ‘completely integrated option’? Certainly, with the widespread adoption of robot-assisted surgery, high-quality outcomes are within the grasp of centres other than elite academic institutions. As techniques develop and experience grows robot-assisted surgery can be increasingly offered, even for resection of more complex tumours.
To ensure that minimally invasive NSS is delivered to the highest standards, it will be necessary for providers to ensure both quality assurance and quality control in their processes. The learning curve needs to be minimised with structured teaching and mentoring, and the use of adjuncts such as intraoperative ultrasonography or fluorescence should be a routine part of care.
Centres offering this technique should be mindful of the well documented volume–outcome relationship that appears to be ubiquitous among complex surgical procedures. If centres are performing less than an optimum number of cases, they may consider affiliating themselves with other such centres in networks and forming a joint clinical governance programme, as has been described for robot-assisted radical prostatectomy and which has shown demonstrable improvements in outcomes.
Finally, auditing and reporting of outcomes remains the cornerstone of quality assurance as shown by the introduction of the BAUS complex surgery audit, which is intended to drive standards of care forward. Publications such as that of Veeratterapillay et al. [1] greatly assist in documenting the progress of new techniques and emerging technologies. Increasingly, patients expect transparency from healthcare providers, and with the necessary support processes in place, such initiatives, and the data that they produce will help to further improve the delivery of complex surgery to patients from all areas of our practice.
* and *†‡
*Division of Cance r Surgery, Peter MacCallum Cancer Centre, †Epworth Healthcare, and ‡Department of Surgery, Central Clinical School, Monash University, Melbourne, Vic., Australia
References
1 Veeratterapillay R, Addla SK, Jelley C et al. Early surgical outcomes and oncological results of robot-assisted partial nephrectomy: a multicentre study. BJU Int 2017; 120: 550–5
2 Uzzo RG, Novick AC. Nephron sparing surgery for renal tumors: indications, techniques and outcomes. J Urol 2001; 166: 6–18
3 Polascik TJ, Pound CR, Meng MV, Partin AW, Marshall FF. Partial nephrectomy: technique, complications and pathological findings. J Urol 1995; 154: 1312–18
4 Gill IS, Meraney AM, Schweizer DK et al. Laparoscopic radical nephrectomy in 100 patients. Cancer 2001; 92: 1843–55
6 Gill IS, Matin SF, Desai MM et al. Comparative analysis of laparoscopic versus open partial nephrectomy for renal tumors in 200 patients. J Urol 2003; 170: 64–8
Article of the Week: Early unclamping technique during RAPN can minimise warm ischaemia without increasing morbidity
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
If you only have time to read one article this week, it should be this one.
Early unclamping technique during robot-assisted laparoscopic partial nephrectomy can minimise warm ischaemia without increasing morbidity
Benoit Peyronnet, Hervé Baumert*, Romain Mathieu, Alexandra Masson-Lecomte†, Yohann Grassano‡, Mathieu Roumiguié§, Walid Massoud*, Vincent Abd El Fattah¶, Franck Bruyère**, Stéphane Droupy¶, Alexandre de la Taille†, Nicolas Doumerc§, Jean-Christophe Bernhard‡, Christophe Vaessen††, Morgan Rouprêt†† and Karim Bensalah
Departments of Urology, University of Rennes, Rennes, *Saint-Joseph Hospital, ††La Pitié Salpétrière Hospital, Paris, †Henri-Mondor Hospital, Créteil, ‡University of Bordeaux, Bordeaux, §University of Toulouse, Toulouse, ¶University of Nimes, Nimes, and **University of Tours, Tours, France
Objective
To compare perioperative outcomes of early unclamping (EUC) vs standard unclamping (SUC) during robot-assisted partial nephrectomy (RAPN), as early unclamping of the renal pedicle has been reported to decrease warm ischaemia time (WIT) during laparoscopic PN.
Patients and Methods
A retrospective multi-institutional study was conducted at eight French academic centres between 2009 and 2013. Patients who underwent RAPN for a renal mass were included in the study. Patients without vascular clamping or for whom the decision to perform a radical nephrectomy was taken before unclamping were excluded. Perioperative outcomes were compared using the chi-squared and Fisher’s exact tests for discrete variables and the Mann–Whitney test for continuous variables. Predictors of WIT and estimated blood loss (EBL) were assessed using multiple linear regression analysis.
Results
In all, there were 430 patients: 222 in the EUC group and 208 in the SUC group. Tumours were larger (35.8 vs 32.3 mm, P = 0.02) and more complex (R.E.N.A.L. nephrometry score 6.9 vs 6.1, P < 0.001) in the EUC group but surgeons were more experienced (>50 procedures 12.2% vs 1.4%, P < 0.001). The mean WIT was shorter (16.7 vs 22.3 min, P < 0.001) and EBL was higher (369.5 vs 240 mL, P = 0.001) in the EUC group with no significant difference in complications or transfusion rates. The results remained the same when analysing subgroups of complex renal tumours (R.E.N.A.L. nephrometry score ≥7) or RAPN performed by less experienced surgeons (<20 procedures). In multivariable analysis, EUC was predictive of decreased WIT (β –0.34; P < 0.001) but was not associated with EBL (β –0.09, P = 0.16).
Conclusions
EUC can reduce WIT during RAPN without increasing morbidity even for complex renal tumours or when being performed by less experienced surgeons.
Article of the Month: An analysis of robot-assisted vs conventional pyeloplasty in children
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
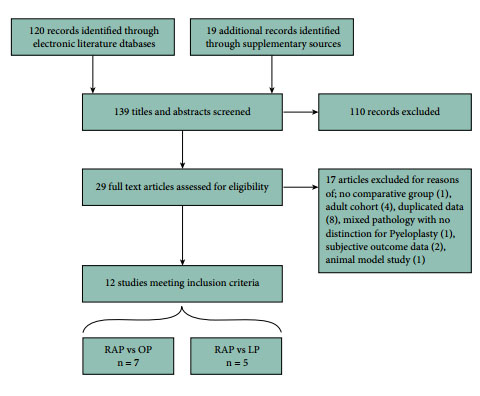
Meta-analysis of robot-assisted vs conventional laparoscopic and open pyeloplasty in children
Thomas P. Cundy*, Leanne Harling†, Archie Hughes-Hallett*†, Erik K. Mayer†, Azad S. Najmaldin‡, Thanos Athanasiou†, Guang-Zhong Yang* and Ara Darzi*†
*The Hamlyn Centre, Institute of Global Health Innovation, and †Department of Surgery and Cancer, St Mary’s Hospital, Imperial College, London; and ‡Department of Paediatric Surgery, Leeds General Infirmary, Leeds, UK
OBJECTIVE
To critically analyse outcomes for robot-assisted pyeloplasty (RAP) vs conventional laparoscopic pyeloplasty (LP) or open pyeloplasty (OP) by systematic review and meta-analysis of published data.
PATIENTS AND METHODS
Studies published up to December 2013 were identified from multiple literature databases. Only comparative studies investigating RAP vs LP or OP in children were included. Meta-analysis was performed using random-effects modelling. Heterogeneity, subgroup analysis, and quality scoring were assessed. Effect sizes were estimated by pooled odds ratios and weighted mean differences. Primary outcomes investigated were operative success, re-operation, conversions, postoperative complications, and urinary leakage. Secondary outcome measures were estimated blood loss (EBL), length of hospital stay (LOS), operating time (OT), analgesia requirement, and cost.
RESULTS
In all, 12 observational studies met inclusion criteria, reporting outcomes of 384 RAP, 131 LP, and 164 OP procedures. No randomised controlled trials were identified. Pooled analyses determined no significant differences between RAP and LP or OP for all primary outcomes. Significant differences in favour of RAP were found for LOS (vs LP and OP). Borderline significant differences in favour of RAP were found for EBL (vs OP). OT was significantly longer for RAP vs OP. Limited evidence indicates lower opiate analgesia requirement for RAP (vs LP and OP), higher total costs for RAP vs OP, and comparable costs for RAP vs LP.
CONCLUSIONS
Existing evidence shows largely comparable outcomes amongst surgical techniques available to treat pelvi-ureteric junction obstruction in children. RAP may offer shortened LOS, lower analgesia requirement (vs LP and OP), and lower EBL (vs OP); but compared with OP, these gains are at the expense of higher cost and longer OT. Higher quality evidence from prospective observational studies and clinical trials is required, as well as further cost-effectiveness analyses. Not all perceived benefits of RAP are easily amenable to quantitative assessment.