Residents’ Podcast: CUA 2018 review
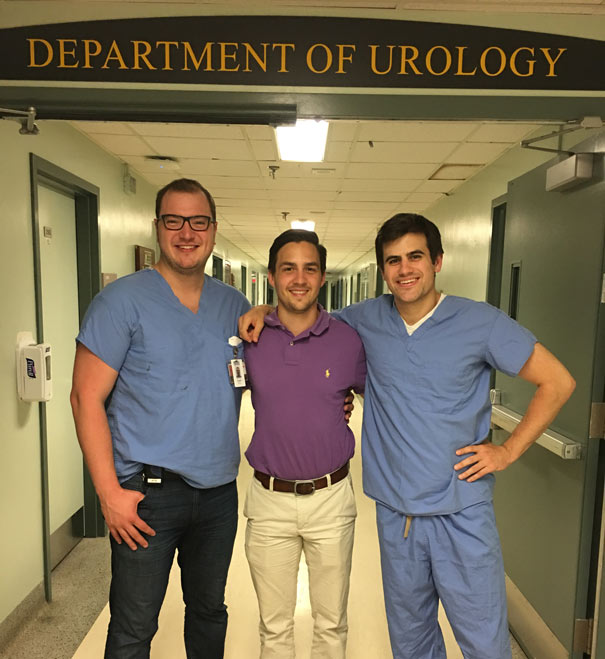
Dalhousie residents Jesse Ory and Andrea Kokorovic sum up the highlights of day 1 at the 2018 Canadian Urological Association annual meeting in Halifax
Song credits
Don’t fear the reaper: Blue oyster cult
Mute city: F Zero
Mortal Kombat Theme: The Immortals
Funky Suspense – Bensound.com