Article of the Week: Value of 111In-PSMA-RGS for salvage lymphadenectomy in recurrent PCa
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
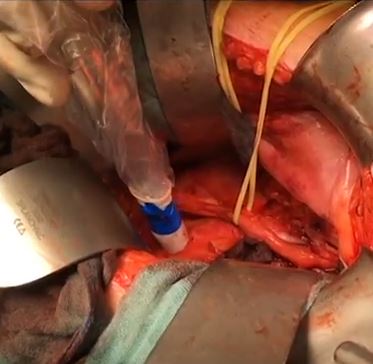
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video discussing the paper.
If you only have time to read one article this week, it should be this one.
Value of 111In-prostate-specific membrane antigen (PSMA)-radioguided surgery for salvage lymphadenectomy in recurrent prostate cancer: correlation with histopathology and clinical follow-up
How to Cite
Rauscher, I., Düwel, C., Wirtz, M., Schottelius, M., Wester, H.-J., Schwamborn, K., Haller, B., Schwaiger, M., Gschwend, J. E., Eiber, M. and Maurer, T. (2017), Value of 111In-prostate-specific membrane antigen (PSMA)-radioguided surgery for salvage lymphadenectomy in recurrent prostate cancer: correlation with histopathology and clinical follow-up. BJU International, 120: 40–47. doi: 10.1111/bju.13713
Abstract
Objectives
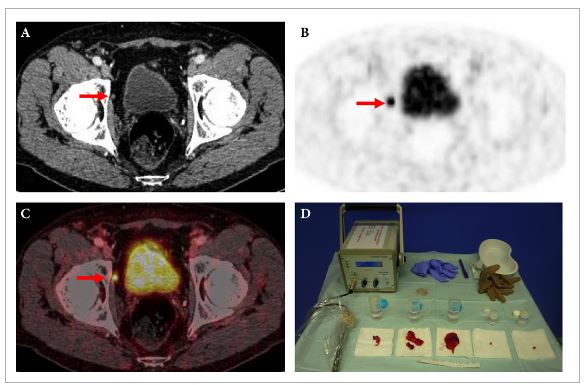
To evaluate the use of 111In-labelled prostate-specific membrane antigen (PSMA)-I&T-based radioguided surgery (111In-PSMA-RGS) for salvage surgery in recurrent prostate cancer (PCa) using comparison of intra-operative gamma probe measurements with histopathological results of dissected specimens. In addition, to determine the success of 111In-PSMA-RGS with regard to postoperative prostate-specific antigen (PSA) responses, PCa-specific treatment-free survival rates and postoperative complication rates.
Patients and Methods
A total of 31 consecutive patients with localized recurrent PCa undergoing salvage surgery with PSMA-targeted radioguided surgery using a 111In-labelled PSMA ligand between April 2014 and July 2015 were retrospectively included in this study. The preoperative (interquartile range; range) median PSA level was 1.3 (0.57–2.53 ng/mL; 0.2–13.9 ng/mL). Results of ex vivo radioactivity rating (positive vs negative) of resected tissue specimens were compared with findings of postoperative histological analysis. Best PSA response without additional treatment was determined after 111In-PSMA-RGS, and salvage-surgery-related postoperative complications and PCa-specific additional treatments were recorded.
Results
In 30/31 patients, 111In-PSMA-RGS allowed intra-operative identification of metastatic lesions. In total, 145 surgical specimens were removed and 51 showed metastatic involvement at histological analysis. According to 111In-PSMA-RGS ex vivo measurements, 48 specimens were correctly classified as metastatic and 87 as cancer-free, four were false-negative and six were false-positive compared with histological evaluation. Follow-up information was available for 30/31 patients. PSA declines of >50% and >90% were observed in 23/30 patients and in 16/30 patients, respectively. In 18/30 patients, a PSA decline to <0.2 ng/mL was observed. In 10/30 patients further PCa-specific treatment was given after a median (range) of 125 (48–454) days post-111In-PSMA-RGS. The remaining 20 patients remained treatment-free at a median (range) follow-up of 337 (81–591) days. Of 30 patients, 10 presented with surgery-related complications (Clavien–Dindo grade 1, n = 6, Clavien–Dindo grade 3b, n = 4).
Conclusion
111In-PSMA-RGS proved to be of high value for intra-operative detection of even small metastatic lesions in patients with PCa scheduled for salvage lymphadenectomy. It allows the exact localization and resection of metastatic tissue during 111In-PSMA-RGS and is therefore anticipated to have a beneficial influence on further disease progression; however, identification of suitable patients on the basis of PSMA-positron-emission tomography imaging as well as clinical variables is essential for satisfactory results to be obtained.