Article of the Week: Natural history of ‘second’ biochemical failure after SRT for PCa
Every Week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this month, it should be this one.Follow us rothwelldouglas for more articles like this one.
Natural history of ‘second’ biochemical failure after salvage radiation therapy for prostate cancer: a multi-institution study
Abstract
Objectives
To describe the natural history of prostate cancer in men who experience a second biochemical recurrence (BCR) after salvage radiotherapy (SRT) after prostatectomy.
Patients and Methods
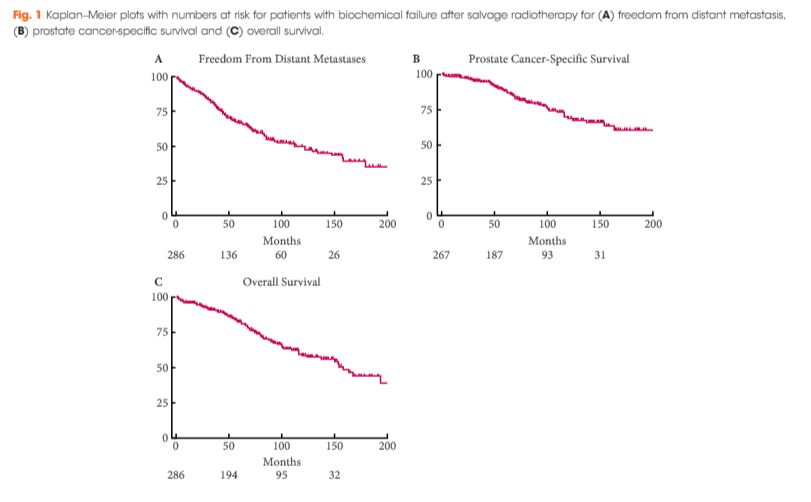
After undergoing SRT at one of two institutions between 1986 and 2013, 286 patients experienced a second BCR, defined as two rises in prostate-specific antigen (PSA) of ≥0.2 ng/mL above nadir. Event rates for distant metastasis (DM) or freedom from DM (FFDM), castration-resistant prostate cancer (CRPC), prostate cancer-specific survival (PCSS), and overall survival (OS) were estimated using the Kaplan–Meier method. Cox regression was used for comparative analyses.
Results
At a median of 6.1 years after second BCR, DM, CRPC, PCSS and OS rates were 41%, 27%, 83% and 73%, respectively. On multivariable analysis, interval to second BCR <1 year (hazard ratio [HR] 2.66, 95% confidence interval [CI] 1.71–4.14; P < 0.001], Gleason score 8–10 (HR 1.65, 95% CI 1.07–2.54; P = 0.022), and concurrent ADT during SRT (HR 1.76, 95% CI 1.08–2.88; P = 0.024) were associated with FFDM, while PCSS was associated with interval to second BCR <1 year (HR 3.00, 95% CI 1.69–5.32; P < 0.001) and concurrent ADT during SRT (HR 2.15, CI 1.13–4.08; P = 0.019). These risk factors were used to stratify patients into three groups, with 6-year FFDM rates of 71%, 59% and 33%, and PCSS rates of 89%, 79%, and 65%, respectively.
Conclusion
Following second BCR after SRT, clinical progression is enriched in a subgroup of patients with prostate cancer, while others remain without DM for long intervals. Stratifying patients into risk groups using prognostic factors may aid counselling and future trial design.