Editorial: Prostate cancer risk prediction and the persistence of uncertainty
Poyet et al. [1] have performed the largest external validation of the European Randomised Study for Screening of Prostate Cancer (ERSPC) and Prostate Cancer Prevention Trial (PCPT) v2.0 risk calculators (RCs) to date, having retrospectively identified 1996 men undergoing prostate biopsy in a Swiss tertiary care facility.
Asides from the validatory nature of this paper [1], there are several other findings though less novel, which are further important additions to the urological literature.
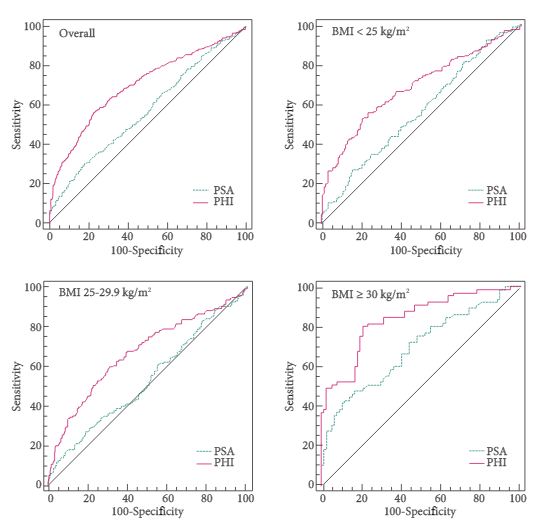
This study confirms the superior discriminative performance of multi-factorial RCs over PSA alone in the assessment of prostate cancer: where the area under the receiver operating characteristic curve (AUC) for the prediction of significant prostate cancer for PSA alone was 0.65, comparing less favourably than 0.73 and 0.70 for the ERSPC and PCPT v2.0 RCs, respectively.
The authors performed sensitivity analysis showing higher detection rates for prostate cancer (29.4% vs 18.1%) and significant prostate cancer (15.9% vs 5.9%) in patients receiving a 12-core biopsy than in those receiving a 6–8 core biopsy.
Supplementary analysis by the authors evaluated the performance of previous versions of the PCPT-RC, specifically v1.0 and PCPT-RC v1.0 with prostate volume. The inclusion of prostate volume demonstrated an improved predictive ability of this RC. The AUC for the prediction of significant prostate cancer using the PCPT-RC v1.0 with prostate volume was 0.74. This contrasts with the ERSPC risk tool: AUC of 0.73 (which includes a trichotomised estimation of prostate volume), and the novel PCPT-RC v2.0; AUC of 0.70 (which does not include prostate volume as a factor).
The authors conclude that the prediction of significant prostate cancer was superior using the ERSPC-RC compared with the PCPT-RC v2.0, in risk thresholds of 8–35%. Their data also shows that the PCPT-RC v2.0 offers a superior net benefit to the ERPSC-RC to a large number of men outside of this range of threshold probabilities. Their findings suggest that the older PCPT-RC v1.0 with prostate volume may offer benefits superior to both the ERSPC and PCPT v2.0 RCs.
The authors assessment of novel risk tools confirms the rationale for guidelines and consensus statements that PSA testing should not be considered on its own, but rather as part of a multivariate approach [2, 3]. This current work suggests that although calibration of risk tools is still not optimal, they offer superior discriminative ability and superior net benefit in identifying patients with significant prostate cancer. This work affirms the role for variables such as DRE, and the importance of prostate volume in addition to PSA in prostate cancer assessment.
Although further refinement of risk tools is necessary, this work encourages confidence in and should garner further traction for the routine use of such tools in the assessment and counselling of patients before prostate biopsy.