The recent article by Tang et al. [1] from the Christie Hospital in Manchester raises an interesting question. The urological cancer plan for England and Wales specifies that review of the pathology of prostate and high-risk superficial bladder cancer should take place as part of the referral process for these cases to specialist pelvic cancer teams, but the penile pathway does not indicate that this is necessary [2]. The Royal College of Pathologists [3] also specifies the need for expert review and/or double reporting in other rare cancers and dysplasias, but does not yet specify this for penile cancers.
Penile cancers are rare, with 600 new cases diagnosed in the UK per year. They are almost invariably squamous cell carcinomas, which also occur at other sites including the lung, upper aerodigestive tract and skin. This may lead some pathologists to assume that they are similar and do not need second opinion or review; however, the subtypes of squamous cell carcinoma that occur on the penis are not common elsewhere, include basaloid, warty and verrucous carcinomas [4], and are not always recognized by general pathologists. The anatomy of the penis is challenging and the identification of invasion of urethra, corpus spongiosum and corpus cavernosum is important in accurate staging. Penile cancers have their own TNM system. TNM7, published in 2010 [5], recognises the importance of grading and different stage groups on prognosis.
Our own experience at St George’s Hospital in South London mirrors that of the Christie Hospital in North West England. Our practice from the outset of the establishment of our supra-regional penile centre was to review outside pathology in the setting of our specialist multidisciplinary meeting to devise a management plan for each patient. We also found that our reviewed cases were more likely to be under-graded and that staging was frequently inaccurate if it was attempted at all. Our original audit was presented at the BAUS annual meeting in 2005. We repeated the audit in 2008 after the publication of the Royal College of Pathologists guidelines on the reporting of penile cancer and found no improvement (unpublished data).
An average urological pathologist in a non-specialist centre in the UK will only see 1–3 cases of penile cancer per year and will have little opportunity or incentive to gain expertise in this area. Although second opinion services through the supra-networks are freely available, these are not always sought, perhaps because of time pressures and the mistaken impression that penile cancers are like those of other sites. There is also a lack of awareness of new entities, for example, differentiated penile intraepithelial neoplasia (PeIN) and subtypes of undifferentiated PeIN. There has been a recent change in nomenclature, whereby all morphological types of squamous carcinoma in situ and dysplasias are now classified within PeIN [6].
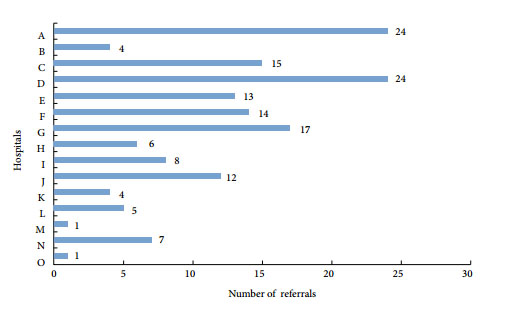
The supra-network of penile centres in the UK has allowed a small group of pathologists to gain expertise in the reporting of penile cancer in a specialist clinical setting, and has produced a group of pathologists with a special interest in this type of tumour, all of whom are seeing at least 25 new cases per year. Many centres are seeing more, with our own centre managing 126 new cases in 2012.
In 2008 we formed a UK-wide group of specialist penile pathologists (the Hobnobs) which meets annually to exchange both clinical and research information and to discuss individual cases. Members of this group are currently updating the Royal College of Pathologists penile guidelines [3]. These will advise central review, but we recognize we are writing them mainly for specialist pathologists to ensure consistent and high-quality assessment of penile cancer to inform the penile cancer team.
In the UK, expert pathological review of penile cancer is already the norm for the penile supra-networks, but it would be difficult to make this the global standard for several reasons. Sub-specialization in penile cancer management is not widely practised outside Britain and there are few specialist high-volume centres, with some notable exceptions in Europe and the USA. Without clinical sub-specialization it is difficult for pathologists to develop an interest and sufficient expertise to offer an expert second opinion because the numbers seen by any individual pathologist will be too small.
The UK penile supra-network system works well and has led to a group of pathologists developing an interest in this area simply because they are seeing a large number of such cases and working with dedicated clinical teams. Penile supra-networks should be adopted worldwide. Following this, a group of expert and experienced pathologists will ultimately be developed, who can offer a central review and expert second opinion service, as has happened over the last 10 years in the UK.
Catherine M. Corbishley
Department of Cellular Pathology, St George’s Healthcare NHS
Trust, London, UK
References
1. Tang V, Clarke L, Gall Z et al. Should centralised histopathological review in penile cancer be the global standard? BJU Int 2014;114: 340–343
2. Manual for Cancer services. Urology measures Version 2.1. NHS National Cancer Peer Review Programme 2011 and Evidence guide for Urology Supraregional Penile MDT NHS National Cancer Peer Review Programme 2010.
3. Royal College of Pathologists. Cancer Datasets and Tissue Pathways. Available at: https://www.rcpath.org/publications-media/publications/datasets.
4. Epstein JI, Cubilla AL, Humphrey PA. Tumours of the Prostate Gland, Seminal Vesicles, Penis and Scrotum. American Registry of Pathology, Washington DC published in collaboration with the Armed Forces Institute of Pathology, 2011, 405–612
5. Gospodarowicz MK (section editor, Genitourinary Tumours). TNM classification of malignant tumours (7th edition) penis. In Edge SB,Byrd DR, Compton CC Fritz AG, Greene FL, Trotti A eds, AJCC Cancer Staging Manual, 7th edn. New York: Springer, 2010:447–455
6. Velazquez EF, Chaux A, Cubilla AL. Histologic classification of penile intraepithelial neoplasia. Semin Diagn Pathol 2012; 29: 96–102