In recent decades, the detection of small renal masses (SRMs) has steadily increased with an accompanying shift of treatment towards partial nephrectomy (PN). Indications for PN have successfully expanded to more challenging cases, and robot-assisted PN (RAPN), in particular, has attracted increasing attention (BJUI, Eur Urol); however, despite excellent cure rates for PN, parallel to the increasing number of patients with SRMs undergoing PN, cases of ipsilateral recurrence after PN are also expected to rise. In addition to the incomplete surgical removal of the primary tumour, unknown multifocality or the development of new tumours or metastasis, in a minority of cases recurrence originates at the previous surgical bed and can be considered a proper local recurrence. Retreatment in these patients represents a specific challenge with radical nephrectomy (RN), ablative treatment, repeat PN, and active surveillance in selected cases as therapeutic options. RN should be considered the least attractive option because of the further damage to renal function that it entails, yet it represents one of the most selected options worldwide. Besides ablative techniques, which should be considered under investigational circumstances only, repeat PN is one of the possible options, especially in cases of recurrences attributable to multifocality or bilateral nature.
Repeat open as well as laparoscopic PN (LPN) have been reported sparsely in the literature, but were shown to be associated with good functional and oncological outcomes given adequate laparoscopic experience and patient selection. Such procedures, however, might be challenging and fraught with complications. The role of repeat RAPN (as well as the role of repeat open PN) in this situation is yet to be defined. Nevertheless, given that current data show RAPN to be a more attractive minimally invasive PN technique compared with its standard laparoscopic counterpart, providing equal or better perioperative outcomes, its advantages may even be greater when repeat PN is indicated.
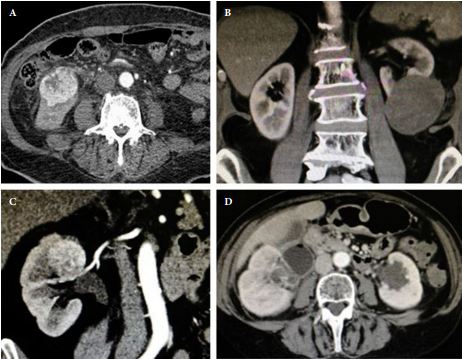
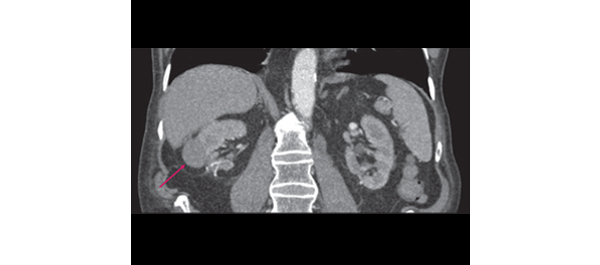
In the current issue of the journal, Autorino et al. report the first study on functional and oncological outcomes and feasibility of repeat RAPN in patients with recurrence after previous PN. Of 490 patients treated with RAPN, nine patients underwent RAPN for recurrent disease at a median time of 39.4 months after previous open or LPN. A total of 12 tumours were removed in these patients, and one third of operations were performed on solitary kidneys. No intra-operative complications were observed, and only two minor complications occurred postoperatively, which were managed conservatively. With regard to functional outcomes, there was a nonsignificant median postoperative decrease in estimated GFR of 7%. More importantly, all patients preserved adequate renal function, which meant that renal replacement therapy was not necessary. With regard to oncological outcomes, all surgical margins were negative and no recurrence was reported.
The results of another study cohort of five patients undergoing repeat RAPN for recurrent disease after open or LPN has recently been published by Jain et al. In their series, surgery was completed in all patients without conversion to RN or an open procedure; furthermore, no complications were reported and the median decrease in GFR was 10%.
Importantly, both series suffer from retrospective evaluation of selective and small sample sizes with a short follow-up, and comparative analysis with other treatment options was not performed; however, the effective comparator for RAPN in this setting has yet to been defined. Bearing in mind current data that demonstrate RAPN to be a preferable minimally invasive PN technique compared with its standard laparoscopic counterparts, the real competitor for RAPN seems to be open surgery. This point was recently also reflected by Mottrie et al. LPN, as a challenging procedure with a long learning curve, limited diffusion and prevalent application in less complex cases, cannot be considered an attractive comparator for RAPN. During the last 8 years, RAPN has become a promising technique which can overcome the technical difficulties of LPN. Three-dimensional vision, ‘endowrist’ technology, and optical magnification allow excellent vision of the operative field and optimum tissue dissection. These technical characteristics help surgeons to minimize ischaemia-time and facilitate accurate tumour excision. Intra-operative ultrasonography, contrast-enhanced sonography, and photodynamic diagnostics can further improve this procedure. It was already shown that the availability of robotic technology is associated with increased use of PN, and, hence, broader diffusion in routine clinical practice may also provide the possibility to outperform results of open PN, even in more complex cases, and will make minimally invasive PN possible and available for more surgeons and patients. Today, the spread of RAPN is only limited by its availability and the associated financial burden. Hence, LPN will currently be considered a cheaper alternative to RAPN in centres with laparoscopic experience and in those which lack the availability of the robot.
Finally, the study from the Cleveland group and the series by Jain et al. provide some valuable support to the feasibility and safety of repeat RAPN and demonstrate that previously performed PN is not a contraindication for RAPN.
Sabine Brookman-May1, Andrea Minervini2, Alessandro Volpe3, Vincenzo Ficarra4, Maciej Salagierski5, Martin Marszalek6,7, Marco Roscigno8, Bülent Akdogan9, Alkuin Vandromme10, Hans Langenhuijsen11, Oscar Rodriguez-Faba12, and Steven Joniau13 for the Renal Cancer Working Group of the Young Academic Urologists (YAU) Working Party of the European Association of Urology (EAU)
1Department of Urology, Ludwig-Maximilians-University, Campus Grosshadern, Munich, Germany, 2Department of Urology, University of Florence, Florence, 3Department of
Urology, University of Eastern Piedmont, Maggiore della Carità Hospital, Novara, 4Department of Oncological and Surgical Sciences, Urologic Unit, University of Padua, Padua,
Italy, 5Department of Urology, Medical University of Łódź, Łódź, Poland, 6Department of Urology and Andrology, Donauspital, Vienna, and 7Department of Urology, Graz Medical University, Graz, Austria, 8Department of Urology, AO Papa Giovanni XXIII, Bergamo, Italy, 9Department of Urology, Hacettepe University, School of Medicine, Ankara, Turkey, 10Klinik für Urologie und Uroonkologie, Klinikum Braunschweig, Germany, 11Laparoscopy, Robotics and Endourology, Radboud University Nijmegen Medical Centre, Nijmegen, The Netherlands, 12Uro-oncology Unit, Fundacio Puigvert, Barcelona, Spain, and 13Department of Urology, University Hospitals Leuven, Leuven, Belgium