Posts
Article of the month: Better QOL with orthotopic neobladders
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Dr. Singh of orthotopic neobladder reconstruction by sigmoid colon.
If you only have time to read one article this week, it should be this one
Prospective comparison of quality-of-life outcomes between ileal conduit urinary diversion and orthotopic neobladder reconstruction after radical cystectomy: a statistical model
Vishwajeet Singh, Rahul Yadav, Rahul Janak Sinha and Dheeraj Kumar Gupta
Department of Urology, King George Medical University, Lucknow, Uttar Pradesh, India
Department of Urology, King George Medical University, Lucknow, Uttar Pradesh, India
OBJECTIVE
• To conduct a prospective comparison of quality-of-life (QoL) outcomes in patients who underwent ileal conduit (IC) urinary diversion with those who underwent orthotopic neobladder (ONB) reconstruction after radical cystectomy for invasive bladder cancers.
PATIENTS AND METHODS
• Between January 2007 and December 2012, 227 patients underwent radical cystectomy and either IC urinary diversion or ONB (sigmoid or ileal) reconstruction.
• Contraindications for ON were impaired renal function (serum creatinine >2 mg/dL), chronic inflammatory bowel disease, previous bowel resection and tumour involvement at the bladder neck/prostatic urethra. Patients who did not have these contraindications chose to undergo either IC or ONB reconstruction, after impartial counselling.
• Baseline characteristics, including demographic profile, body mass index, comorbidities, histopathology of the cystoprostatectomy (with lymph nodes) specimen, pathological tumour stage, postoperative complications, adjuvant therapy and relapse, were recorded and compared.
• The European Organization for Research and Treatment of Cancer QoL questionnaire C30 version 3 was used to analyse QoL before surgery and 6, 12 and 18 months after surgery.
RESULTS
• Of the 227 patients, 28 patients in the IC group and 35 in the ONB group were excluded. The final analysis included 80 patients in the IC and 84 in the ONB group.
• None of the baseline characteristics were significantly different between the groups, except for age, but none of the baseline QoL variables were found to be correlated with age.
• In the preoperative phase, there were no significant differences in any of the QoL domains between the IC or the ONB groups. At 6, 12 and 18 months in the postoperative period, physical functioning (P < 0.001, P < 0.001 and P = 0.001, respectively), role functioning (P = 0.01, P = 0.01 and P = 0.003, respectively), social functioning (P = 0.01, P = 0.01 and P = 0.01, respectively) and global health status/QoL (P < 0.001, P < 0.001 and P = 0.002, respectively) were better in patients in the ONB group than in those in the IC group and the differences were significant.
• The financial burden related to bladder cancer treatment was significantly lower in the ONB group than in the IC group at 6, 12 and 18 months of follow-up (P = 0.05, P = 0.05 and P = 0.005, respectively)
CONCLUSIONS
• ONB is better than IC in terms of physical functioning, role functioning, social functioning, global health status/QoL and financial expenditure.
• ONB reconstruction provides better QoL outcomes than does IC urinary diversion.
Editorial: Life is good with orthotopic bladder substitutes!
In the present issue of the BJUI, Singh et al. [1] present the results of a non-randomized prospective study comprising 80 patients who underwent ileal conduit diversion and 84 who underwent orthotopic bladder substitution. Quality of life was assessed using the European Organisation for the Research and Treatment of Cancer quality-of-life questionnaire, the QLQ-30C, at 6, 12 and 18 months postoperatively. Physical and social functioning and global health status were significantly better in patients with orthotopic bladder substitution than in those who underwent ileal conduit diversion. Moreover, the postoperative financial burden was significantly lower for patients in the orthotopic bladder group than for those in the ileal conduit group, who required stoma appliances, a finding of particular importance not only in India, where the study was performed, but worldwide. The authors’ results are particularly impressive given their use of a questionnaire that included many items (‘Were you short of breath?’, ‘Did you need to rest?’, ‘Have you lacked appetite?’, ‘Have you been constipated?’, ‘Did you feel tense?’, ‘Did you worry’ or ‘Did you feel irritable?’, etc.) that can hardly discriminate between the quality of life of patients who underwent orthotopic bladder substitution and those who underwent ileal conduit diversion. To find significant differences between the two types of urinary diversion, despite such dilution factors, speaks strongly in favour of orthotopic bladder substitution.
The results of this prospective single-centre trial are of particular importance because, as the authors state, other investigators could not show such differences, presumably for a variety of reasons, such as too few patients or single follow-up assessments given at time points that varied from patient to patient. Quality-of-life assessment at similar follow-up time points, as performed by these authors, is important because, with adequate counselling, the postoperative function of orthotopic bladder substitutes improves over time.
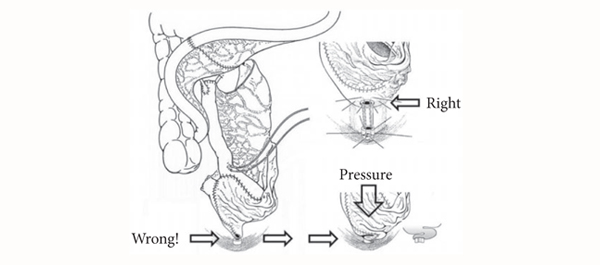
Without a doubt, however, a poorly functioning orthotopic bladder substitute may lead to a poorer quality of life than a well-functioning ileal conduit diversion. Poor functional results and life-threatening complications can be largely avoided with ileal orthotopic bladder substitutes, provided the treating urologist has adequate knowledge of the procedure and the patient receives adequate postoperative education [2]. The major ways to ensure good results are:
- appropriate patient selection (good renal function, regular follow-up possible);
- the avoidance of damage to the sphincter apparatus and its innervation (individualized nerve-sparing cystectomy, minimum use of bipolar electrocautery near the pelvic plexus and membranous urethra);
- the use of ileum instead of colon (better compliance) [3-5];
- the avoidance of a funnel-shaped outlet that can result in kinking, outlet obstruction, residual infected urine and, in the worst case, lifelong need for clean intermittent catheterization (CIC) (Fig. 1).
By contrast to most other urological procedures, orthotopic bladder substitution requires proactive postoperative management [6] to ensure:
- residual urine-free spontaneous voiding after catheter removal;
- sterile urine to improve urinary continence and to reduce mucous production [7];
- the prevention of salt loss syndrome and metabolic acidosis by increased salt intake and sodium bicarbonate substitution in the early postoperative period to ensure a base excess of +2;
- a systematic increase in functional capacity by progressively expanding voiding intervals to obtain a reservoir capacity of ∼500 mL and, thus, a low end-fill pressure which ensures urinary continence day and night (the latter combined with the use of an alarm clock).
It is equally important to perform lifelong follow-up of patients and regularly at 6- to 12-month intervals so as to diagnose and treat early secondary complications, such as uretero-intestinal strictures or residual, infected urine. If the latter occurs, any form of outlet obstruction, such as ileal mucosa protruding in front of the bladder outlet, strictures or growth of inadvertently left prostatic tissue, must be looked for and treated. In our own experience, secondary outlet obstruction occurred in ∼20% of patients observed for 10 years. This rather high incidence is typical for intestinal bladder substitutes because when voiding, unlike the genuine bladder, there is no coordinated contraction of the reservoir wall which would result in an elevated voiding pressure which, in turn, would overcome an outlet resistance. Bladder substitutes empty mainly by gravitational force alone. If voiding is only possible by abdominal straining, then something must be wrong; therefore, instead of recommending CIC for patients who build up residual and consecutively infected urine, we strongly favour treating the outlet obstruction, usually on an outpatient basis. The avoidance of the need for CIC through surgical technique (no funnel-shaped outlet) and during regular follow-up by treating any potential cause of residual urine can substantially improve the patient’s quality of life. It also avoids the cost of catheters and the risk of infectious complications. Thanks to this active management and removal of any outlet obstruction, 96% of our patients followed for 10 years were still able to void spontaneously [8].
Urs E. Studer
Department of Urology, University Hospital Bern, Bern, Switzerland
References
- Singh V, Yadav R, Sinha RJ, Gupta DK. Prospective comparison of quality-of-life outcomes between ileal conduit urinary diversion and orthotopic neobladder reconstruction after radical cystectomy: a statistical model. BJU Int 2014; 113: 726–732
- Thurairaja R, Burkhard FC, Studer UE. The orthotopic neobladder. BJU Int 2008; 102: 1307–1313
- Berglund B, Kock NG, Myrvold HE. Volume capacity and pressure characteristics of the continent cecal reservoir. Surg Gynecol Obstet 1986; 163: 42–48
- Schrier BP, Laguna MP, van der Pal F, Isorna S, Witjes JA. Comparison of orthotopic sigmoid and ileal neobladders: continence and urodynamic parameters. Eur Urol 2005; 47: 679–685
-
Paananen I, Ohtonen P, Perttilä I et al. Functional results after orthotopic bladder substitution: a prospective multicenter study comparing four types of neobladder. Scand J Urol 2014; 48: 90–98
- Varol C, Studer UE. Managing patients after an ileal orthotopic bladder substitution. BJU Int 2004; 93: 266–270
- Zehnder P, Dhar N, Thurairaja R, Ochsner K, Studer UE. Effect of urinary tract infection on reservoir function in patients with ileal bladder substitute. J Urol 2009; 181: 2545–2549
- Thurairaja R, Studer UE. How to avoid clean intermittent catheterization in men with ileal bladder substitution. J Urol 2008; 180: 2504–2509
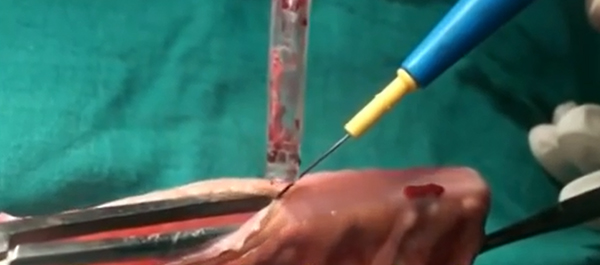
Video: Orthotopic neobladder reconstruction by sigmoid colon
Prospective comparison of quality-of-life outcomes between ileal conduit urinary diversion and orthotopic neobladder reconstruction after radical cystectomy: a statistical model
Vishwajeet Singh, Rahul Yadav, Rahul Janak Sinha and Dheeraj Kumar Gupta
Department of Urology, King George Medical University, Lucknow, Uttar Pradesh, India
OBJECTIVE
• To conduct a prospective comparison of quality-of-life (QoL) outcomes in patients who underwent ileal conduit (IC) urinary diversion with those who underwent orthotopic neobladder (ONB) reconstruction after radical cystectomy for invasive bladder cancers.
PATIENTS AND METHODS
• Between January 2007 and December 2012, 227 patients underwent radical cystectomy and either IC urinary diversion or ONB (sigmoid or ileal) reconstruction.
• Contraindications for ON were impaired renal function (serum creatinine >2 mg/dL), chronic inflammatory bowel disease, previous bowel resection and tumour involvement at the bladder neck/prostatic urethra. Patients who did not have these contraindications chose to undergo either IC or ONB reconstruction, after impartial counselling.
• Baseline characteristics, including demographic profile, body mass index, comorbidities, histopathology of the cystoprostatectomy (with lymph nodes) specimen, pathological tumour stage, postoperative complications, adjuvant therapy and relapse, were recorded and compared.
• The European Organization for Research and Treatment of Cancer QoL questionnaire C30 version 3 was used to analyse QoL before surgery and 6, 12 and 18 months after surgery.
RESULTS
• Of the 227 patients, 28 patients in the IC group and 35 in the ONB group were excluded. The final analysis included 80 patients in the IC and 84 in the ONB group.
• None of the baseline characteristics were significantly different between the groups, except for age, but none of the baseline QoL variables were found to be correlated with age.
• In the preoperative phase, there were no significant differences in any of the QoL domains between the IC or the ONB groups. At 6, 12 and 18 months in the postoperative period, physical functioning (P < 0.001, P < 0.001 and P = 0.001, respectively), role functioning (P = 0.01, P = 0.01 and P = 0.003, respectively), social functioning (P = 0.01, P = 0.01 and P = 0.01, respectively) and global health status/QoL (P < 0.001, P < 0.001 and P = 0.002, respectively) were better in patients in the ONB group than in those in the IC group and the differences were significant.
• The financial burden related to bladder cancer treatment was significantly lower in the ONB group than in the IC group at 6, 12 and 18 months of follow-up (P = 0.05, P = 0.05 and P = 0.005, respectively)
CONCLUSIONS
• ONB is better than IC in terms of physical functioning, role functioning, social functioning, global health status/QoL and financial expenditure.
• ONB reconstruction provides better QoL outcomes than does IC urinary diversion.