Article of the Week: Frozen Section During Partial Nephrectomy: Does it Predict Positive Margins?
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Frozen Section During Partial Nephrectomy: Does it Predict Positive Margins?
OBJECTIVE
To investigate the clinical utility of frozen section (FS) analysis performed during partial nephrectomy (PN) and its influence on intra-operative management.
PATIENTS AND METHODS
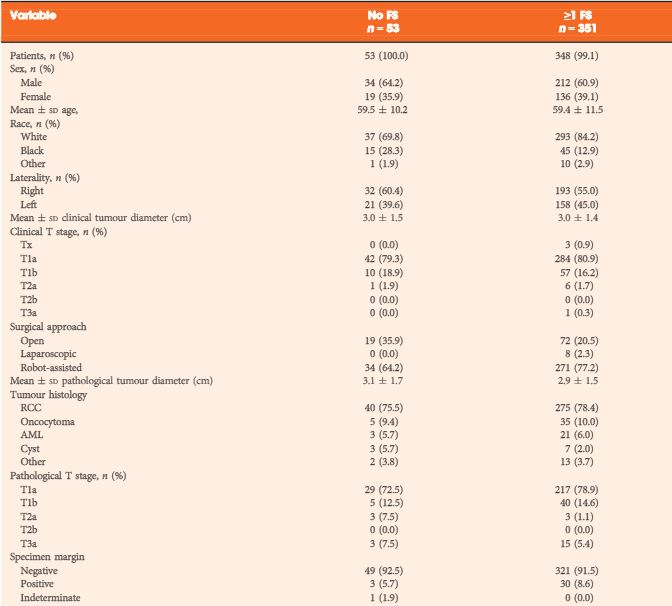
We performed a retrospective analysis of consecutive PN cases from 2010 to 2013. We evaluated the concordance between the intra-operative FS diagnosis and the FS control diagnosis, a postoperative quality assurance measure performed on all FS diagnoses after formalin fixation of the tissue. We also evaluated the concordance between the intra-operative FS diagnosis and the final specimen margin. Operating reports were reviewed for change in intra-operative management for cases with a positive or atypia FS diagnosis, or if the mass was sent for FS.
RESULTS
A total of 576 intra-operative FSs were performed in 351 cases to assess the PN tumour bed margin, 19 (5.4%) of which also had a mass sent for FS to assess the tumour type. The concordance rate between the FS diagnosis and the FS control diagnosis was 98.3%. There were 30 (8.5%) final positive specimen margins, of which four (13.3%) were classified as atypia, 17 (56.7%) as negative and nine (30%) as positive on FS diagnosis. Intra-operative management was influenced in six of nine cases with a positive FS diagnosis and in one of nine cases with an FS diagnosis of atypia.
CONCLUSIONS
The relatively high false-negative rate, controversy over the prognosis of a positive margin, and inconsistency in influencing intra-operative management are arguments against the routine use of FS in PN cases.