Posts
Article of the week: Deep learning computer vision algorithm for detecting kidney stone composition
Every week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
If you only have time to read one article this week, we recommend this one.
Deep learning computer vision algorithm for detecting kidney stone composition
Kristian M. Black*, Hei Law†, Ali Aldoukhi*, Jia Deng† and Khurshid R. Ghani*
*Department of Urology, University of Michigan, Ann Arbor, MI, and †Department of Computer Science, Princeton University, Princeton, NJ, USA
Abstract
Objectives
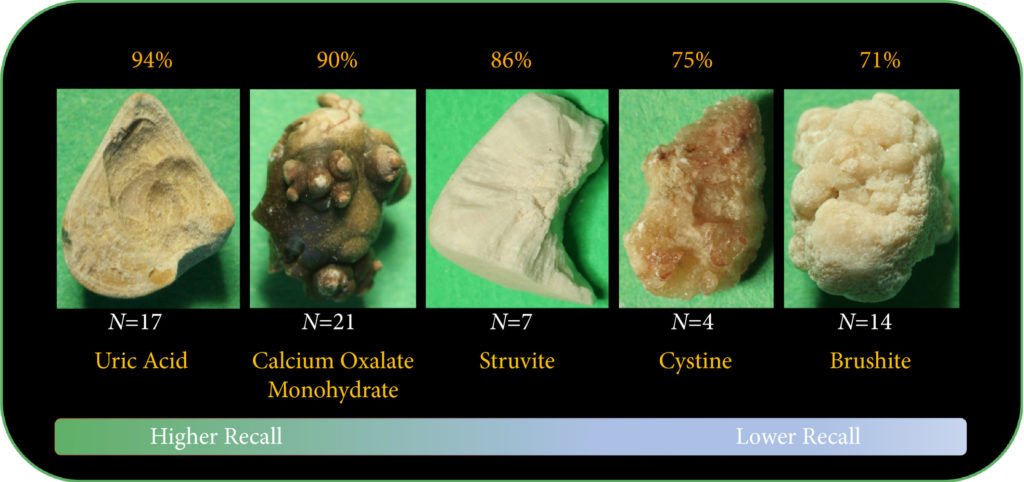
To assess the recall of a deep learning (DL) method to automatically detect kidney stones composition from digital photographs of stones.
Materials and Methods
A total of 63 human kidney stones of varied compositions were obtained from a stone laboratory including calcium oxalate monohydrate (COM), uric acid (UA), magnesium ammonium phosphate hexahydrate (MAPH/struvite), calcium hydrogen phosphate dihydrate (CHPD/brushite), and cystine stones. At least two images of the stones, both surface and inner core, were captured on a digital camera for all stones. A deep convolutional neural network (CNN), ResNet‐101 (ResNet, Microsoft), was applied as a multi‐class classification model, to each image. This model was assessed using leave‐one‐out cross‐validation with the primary outcome being network prediction recall.
Results
The composition prediction recall for each composition was as follows: UA 94% (n = 17), COM 90% (n = 21), MAPH/struvite 86% (n = 7), cystine 75% (n = 4), CHPD/brushite 71% (n = 14). The overall weighted recall of the CNNs composition analysis was 85% for the entire cohort. Specificity and precision for each stone type were as follows: UA (97.83%, 94.12%), COM (97.62%, 95%), struvite (91.84%, 71.43%), cystine (98.31%, 75%), and brushite (96.43%, 75%).
Conclusion
Deep CNNs can be used to identify kidney stone composition from digital photographs with good recall. Future work is needed to see if DL can be used for detecting stone composition during digital endoscopy. This technology may enable integrated endoscopic and laser systems that automatically provide laser settings based on stone composition recognition with the goal to improve surgical efficiency.
Article of the week: Early and rapid prediction of postoperative infections following PCNL in patients with complex kidney stones
Every week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an editorial and a visual abstract prepared by prominent members of the urological community. These are intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
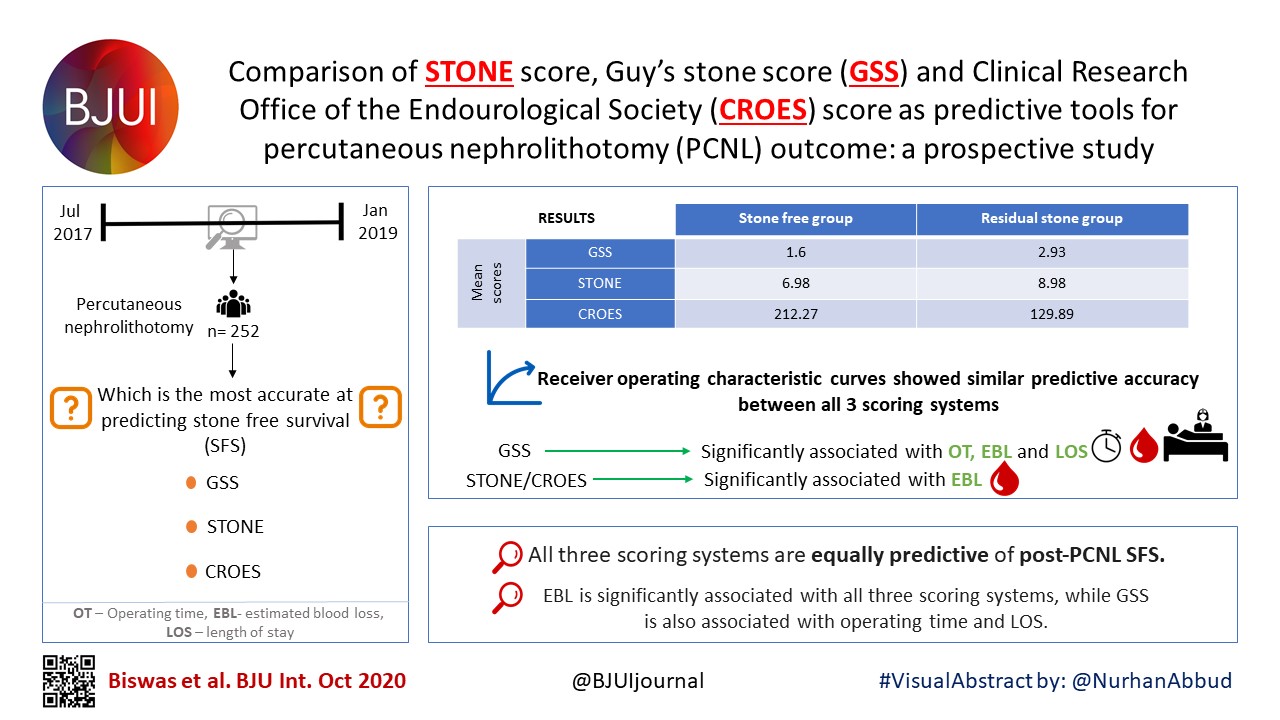
Early and rapid prediction of postoperative infections following percutaneous nephrolithotomy in patients with complex kidney stones
Dong Chen*, Chonghe Jiang†, Xiongfa Liang*, Fangling Zhong*, Jian Huang*, Yongping Lin‡, Zhijian Zhao*, Xiaolu Duan*, Guohua Zeng* and Wenqi Wu*
*Department of Urology, Guangdong Key Laboratory of Urology, Minimally Invasive Surgery Center, The First Affiliated Hospital of Guangzhou Medical University, Guangzhou, †Department of Urology, The People’s Hospital of Qingyuan City, The Sixth Affiliated Hospital of Guangzhou Medical University, Qingyuan, and ‡Department of Laboratory Medicine, The First Affiliated Hospital of Guangzhou Medical University, Guangzhou, Guangdong, China
Abstract
Objectives
To obtain more accurate and rapid predictors of postoperative infections following percutaneous nephrolithotomy (PCNL) in patients with complex kidney stones, and provide evidence for early prevention and treatment of postoperative infections.
Patients and Methods
A total of 802 patients with complex kidney stones who underwent PCNL, from September 2016 to September 2017, were recruited. Urine tests, urine cultures (UCs) and stone cultures (SCs) were performed, and the perioperative data were prospectively recorded.
Results
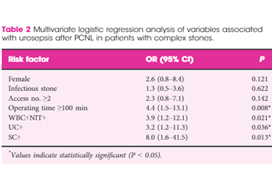
In all, 19 (2.4%) patients developed postoperative urosepsis. A multivariate logistic regression analysis revealed that an operating time of ≥100 min, urine test results with both positive urine white blood cells (WBC+) and positive urine nitrite (WBC+NIT+), positive UCs (UC+), and positive SCs (SC+) were independent risk factors of urosepsis. The incidence of postoperative urosepsis was higher in patients with WBC+NIT+ (10%) or patients with both UC+ and SC+ (UC+SC+; 8.3%) than in patients with negative urine test results or negative cultures (P < 0.01). Preoperative WBC+NIT+ was predictive of UC+SC+, with an accuracy of >90%. The main pathogens found in kidney stones were Escherichia coli (44%), Proteus mirabilis (14%) and Staphylococcus (7.4%); whilst the main pathogens found in urine were E. coli (54%), Enterococcus (9.4%) and P. mirabilis (7.6%). The incidence of E. coli was more frequent in the group with urosepsis than in the group without urosepsis (P < 0.05).
Conclusions
WBC+NIT+ in preoperative urine tests could be considered as an early and rapid predictor of UC+SC+ and postoperative urosepsis. Urosepsis following PCNL was strongly associated with E. coli infections in patients with complex kidney stones.
Editorial: Predicting sepsis after percutaneous nephrolithotomy
In this month’s BJUI, Chen et al. [1] report on a large series of percutaneous nephrolithotomy (PCNL) procedures from Guangzhou in China. The authors studied patients who developed postoperative urosepsis and looked for any predictive factors that would herald impending sepsis.
In this latest report, the authors analysed 802 patients with complex kidney stones undergoing PCNL in a single centre. ‘Complex’ was defined as complete staghorn, partial staghorn or pelvic stone with at least two calyceal stones. Midstream urines (MSU) were collected and analysed for white blood cells (WBC) and nitrites (NIT). Antibiotics were given preoperatively if the urine culture (UC) was positive for WBC (WBC+) or NIT (NIT+). Standard single‐dose antibiotic was given on induction of anaesthesia and only continued for 48 h if the culture was positive. Stone cultures (SCs) were routinely collected. Of the 802 patients, UCs were positive (UC+) in 171 (21%) and SCs subsequently positive (SC+) in 30%. Postoperatively, 98 (12%) developed a fever, 62 (7.7%) developed systemic inflammatory response syndrome (SIRS), and 19 (2.4%) developed sepsis as defined by the quick Sequential (sepsis‐related) Organ Failure Assessment (qSOFA).
Multiple factors were significantly associated with sepsis: female sex (79% vs 40%), infection stone (47% vs 21%), long operating time ≥100 min (74% vs 45%), multiple accesses (32% vs 10%), UC+ (63% vs 20%), SC+ (89% vs 29%), fever (74% vs 11%), as well as being both WBC+ and NIT+ (63% vs 13%). Conversely, if WBC and NIT were negative (WBC–NIT–) the risk of sepsis was only 5.3%. On multivariate analysis SC+ (odds ratio [OR] 8.0), operating time ≥100 min (OR 4.4), WBC+ and NIT+ (OR 3.9), UC+ (OR 3.2), were independent risk factors for sepsis. Not surprisingly having UC+, SC+ or both showed a statistically higher incidence of fever, SIRS, and sepsis. Being WBC+ and NIT+ was the best predictor of having both UC+ and SC+ with an impressive 92% sensitivity and 98% specificity.* Similarly, WBC+ and NIT+ was the best predictor of sepsis with 92% sensitivity and 82% specificity. The absolute risk of sepsis was only 0.2% if WBC–NIT–, 2.8% if only one was positive, and 10% if WBC+NIT+.
The authors also report on the bacterial findings of the UCs and SCs. In the SCs, Escherichia coli (44%), Proteus mirabilis (14%) and Staphylococcus (7.4%) were the most common; whilst in the UCs, E. coli (54%), Enterococcus (9.4%) and P. mirabilis (7.6%) were predominant. It is important to remember the potential differences when interpreting UCs preoperatively and to ensure broad‐spectrum cover is given and this justifies the sending of SCs, particularly in high‐risk patients [1].
The recognition of early sepsis is paramount and has been recognised in previous studies leading to the ‘golden hour’, when early aggressive treatment of the infection has been shown to lead to better outcomes [2]. In a large study by Kumar et al. [2], early antimicrobial administration (within the first hour of hypotension from septic shock) led to a higher overall survival; but worryingly, only 50% of patients received appropriate antibiotics within 6 h. Thus, if high‐risk patients could be predicted then closer monitoring, aggressive fluid management, and early broad‐spectrum antibiotics with intensive care support could be targeted at those specific patients.
There are multiple definitions for infection, e.g., sepsis, severe sepsis, septic shock, and SIRS. The 2016 International Consensus attempted to clarify these and defined sepsis as ‘A life‐threatening organ dysfunction due to dysregulated host response to infection’ [3]. They found the term ‘severe sepsis’ to be obsolete. Septic shock is defined as ‘a subset of sepsis in which particularly profound circulatory, cellular, and metabolic abnormalities are associated with a greater risk of mortality than with sepsis alone’ [3]. The Consensus recommended organ dysfunction is assessed by a SOFA score increase of ≥2, as this is associated with a mortality of 10%. This then led to the bedside assessment clinical score called qSOFA. Poorer outcomes were associated with two or more of the qSOFA criteria: respiratory rate ≥22 breaths/min, altered mentation (as judged by the Glasgow Coma Scale), and systolic blood pressure ≤100 mmHg.
In this current study [1], many of the factors associated with postoperative sepsis are logical and have been demonstrated before, e.g., female sex, infection stone, prolonged operating times, and multiple accesses. This paper has shown that careful attention to the preoperative urine dipstick can provide important prediction of potential severe infective complications postoperatively. In an era of antibiotic stewardship this could help guide targeted preoperative and prolonged postoperative antibiotics for a small group of patients, whilst managing WBC–NIT– patients with standard prophylaxis only. The high‐risk group should also be observed very closely postoperatively and moved to a high‐dependence setting rapidly if clinical signs of sepsis develop. It would also suggest that in this high‐risk group, operating times and intra‐renal pressure should be minimised. It may be that in these patients it is better to use larger tract PCNL sizes to allow rapid fragmentation and evacuation of the stone and that consideration should be given to staged procedures in complicated stones where multiple access is being considered to minimise operating time and allow analysis of intraoperative SCs.
It should of course be remembered that antibiotic decisions should be based on local policies and sensitivities, which may be very different from this population. Rapid treatment of sepsis is paramount and the most recent ‘Hour‐1’ bundle provides the most up‐to‐date guidance for immediate resuscitation and management with lactate management, blood cultures, broad‐spectrum antibiotics, i.v. fluids, and early use of vasopressors if the blood pressure does not respond to fluid replacement [4].
by Matt Bultitude and Kay Thomas
References
- , , et al. Early and rapid prediction for postoperative infections following percutaneous nephrolithotomy in patients with complex kidney stones. BJU Int 2019; 123: 1041– 7
- , , et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med 2006; 34: 1589– 96
- , , et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis‐3). JAMA 2016; 315: 801– 10
- , , . The surviving sepsis campaign bundle: 2018 update. Crit Care Med 2018; 46: 997– 1000
Article of the Month: Surgical outcomes of PCNL and results of stone analysis
Every Month the Editor-in-Chief selects an Article of the Month from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Surgical outcomes of percutaneous nephrolithotomy in 3402 patients and results of stone analysis in 1559 patients
*, *, *, *, * and †
*Departments of Urology, and †Pathology, Sindh Institute of Urology and Transplantation, Civil Hospital, Karachi, Pakistan
Abstract
Objective
To report our experience of a series of percutaneous nephrolithotomy (PCNL) procedures in a single centre over 18 years in terms of patient and stone characteristics, indications, stone clearance and complications, along with the results of chemical analysis of stones in a subgroup.
Patients and Methods
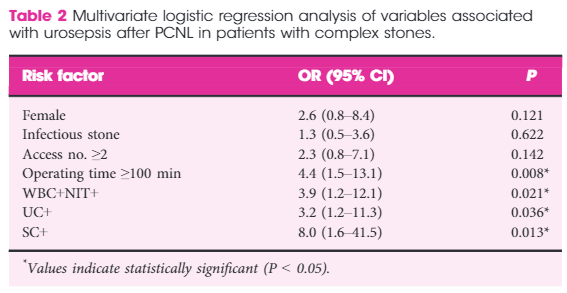
We retrospectively analysed the outcomes of PCNL in 3402 patients, who underwent the procedure between 1997 and 2014, obtained from a prospectively maintained database. Data analysis included patients’ age and sex, laboratory investigations, imaging, punctured calyx, duration of operation, volume of irrigation fluid, radiation exposure time, blood transfusion, complications and stone-free status at 1-month follow-up. For the present analysis, outcomes in relation to complications and success were divided in two eras, 1997–2005 and 2006–2014, to study the differences.
Results
Of the 3402 patients, 2501 (73.5%) were male and 901 (26.5%) were female, giving a male:female ratio of 2.8:1. Staghorn (partial or complete) calculi were found in 27.5% of patients, while 72.5% had non-staghorn calculi. Intracorporeal energy sources used for stone fragmentation included ultrasonography in 917 patients (26.9%), pneumatic lithoclast in 1820 (53.5%), holmium laser in 141 (4.1%) and Lithoclast® master in 524 (15.4%). In the majority of patients (97.4%) a 18–22-F nephrostomy tube was placed after the procedure, while 69 patients (2.03%) underwent tubeless PCNL. The volume of the irrigation fluid used ranged from 7 to 37 L, with a mean of 28.4 L. The stone-free rate after PCNL in the first era studied was 78%, vs 83.2% in the second era, as assessed by combination of ultrasonography and plain abdominal film of the kidney, ureter and bladder. The complication rate in the first era was 21.3% as compared with 10.3% in the second era, and this difference was statistically significant. Stone analysis showed pure stones in 41% and mixed stones in 58% of patients. The majority of stones consisted of calcium oxalate.
Conclusions
This is the largest series of PCNL reported from any single centre in Pakistan, where there is a high prevalence of stone disease associated with infective and obstructive complications, including renal failure. PCNL as a treatment method offers an economic and effective option in the management of renal stone disease with acceptable stone clearance rates in a resource-constrained healthcare system.
Editorial: Management of urolithiasis in South Asia
The article by Rizvi et al. [1] makes a great read. The authors deserve credit for their work and the data presented. A few points merit mention to summarise and put the article in perspective.
First, the authors present a mammoth database from a public sector hospital in Pakistan. In the initial era, as noted by the authors, they adopted extracorporeal shockwave lithotripsy (ESWL) as their mainstay for treating stones. ESWL as the least invasive, safe and readily available method remained the preferred option initially. However, stones seen in South Asia differ from those in the West. In this geographical area, the stone bulk is large and often not amenable to ESWL. In the subsequent period, the authors changed to percutaneous surgery. The reason for this shift, apart from large stone burden, may also have been influenced by local facto required to be travelled by patients to reach a healthcare facility and the lack of resources and infrastructure in remote locations. In such situations, the treatment option that offers rapid, safe, and efficacious results would be preferred. These criteria are fulfilled with the percutaneous approach to renal stones and this is what the authors did!
Second, it is worthwhile noting that that the need for embolisation and/or nephrectomy is a miniscule number in this series [1]. This emphasises the importance of the basic tenet in percutaneous renal surgery that a perfect initial access is the secret to successful percutaneous removal of stones. It should be noted that in this large series the complications across all Clavien–Dindo complication grades reduced as the authors ascended the learning curve.
Third, we feel the major limitation of this study [1] was the means of assessing the stone-free rate. The authors used a combination of ultrasonography and plain abdominal radiograph of the kidneys, ureters and bladder. As acknowledged by the authors this could have possibly overestimated the stone-free rates and skewed the data and interpretation. The authors can substantiate these findings in further prospective studies.
Fourth, the paper exemplifies that stone composition, choice of approach, and patient preferences vary from region to region globally. The findings in the study [1] are similar to the results of Desai et al. [2] from India.
Last but not the least, the AUA guidelines [3] state that the optimal strategy for stone management must take into consideration patient health and economic outcomes. Stone-free requirement is global but economic implications are regional. In this context, the treatment options for similar sized stones may vary for a particular patient located in Europe or Asia. Hence, we feel this paper could be considered as a benchmark for future multicentre trials investigating treatment options and strategies for urolithiasis in South Asia.
and
Department of Urology, Muljibhai Patel Urological Hospital, Nadiad, Gujarat, India
References
1 Rizvi SA, Hussain M, Askari SH, Hashmi A, Lal M, Zafar MN. Surgical outcomes of percutaneous nephrolithotomy in 3402 patients and results of stone analysis in 1559 patients from a single centre in Pakistan. BJUInt 2017; 120: 702–9
2 Desai M, Jain P, Ganpule A, Sabnis R, Patel S, Shrivastav P. Developments in technique and technology: the effect on the results of percutaneous nephrolithotomy for staghorn calculi. BJU Int 2009; 104:542–8
3 Assimos D, Krambeck A, Miller NL et al. Surgical management of stones: American Urological Association/Endourological Society Guideline. Available at: https://www.auanet.org/guidelines/surgical-management-of-stones-(aua/endourological-society-guideline-2016). Accessed August 2017
Royal Society of Medicine: Key issues in Endourology
The RSM section of Urology #RSMUrology hosted a day on the Key issues in Endourology on 20th October. This was the first meeting of the academic year under President Roland Morley. Sri Sriprisad put together a complete endourology day with key subject areas of “PCNL and stones”, “upper tract TCC” and “BPH and retention”. Speakers from India, America and Spain provided expert opinions from around the globe.
The day started with the evolution of stone and urological laparoscopic surgery. Showing an insight into the challenges with the initial introduction of laparoscopic urological surgery. In order to allow surgeons the chance to discuss their experiences and troubleshoot and develop surgical techniques the SLUG forum (southern laparoscopic urology group) was created, which is still running today in the annual AUA meeting.
PCNL techniques were the subject for several debate lectures. Access for PCNL tracts was debated by Dr Janak Desai, visiting from Samved Urology hospital in India, arguing for fluoroscopic puncture with over 10,000 cases to date! Jonathan Glass, from Guy’s and St. Thomas’ Hospital, spoke for the prone position for the majority of PCNL, but selecting the supine position in 5-10% of cases depending on the anatomy and stone position. Dr Desai also spoke on ultra-mini PCNL, which he advocates using to treat solitary kidney stones under 2 cm in preference to flexible ureteroscopy.
The future of ESWL was debated and the audience voted that it is still “alive and clicking” by a narrow margin. However, although up to 80% clearance rates are quoted for upper pole stones less than 2 cm, the problem is that results of treatment are varied and unpredictable, and real-life success rates are far inferior. The variation in results may in part be due to the fact that there are no formal training courses for specialist radiographers nor SAC requirements for specialist registrars. Professor Sam McClinton presented on clinical research in stone disease with results from the TISU trial on primary ESWL vs. ureteroscopy for ureteric stones due out next year. The results will be fascinating and may help to decide if ESWL has a future in the UK.
Professor Margaret Pearle, visiting from the University of Texas Southwestern Medical Centre, explained the importance of treating residual fragments. With data showing that 20 – 36% of >2 mm residual stones after ureteroscopy required repeat surgery within 1 year. In a thought provoking lecture, she presented data showing that ureteroscopy may not be as good as we think and when critically examined, true stone-free rates maybe no better than ESWL. Maybe miniaturised PCNL is the way forward after all?
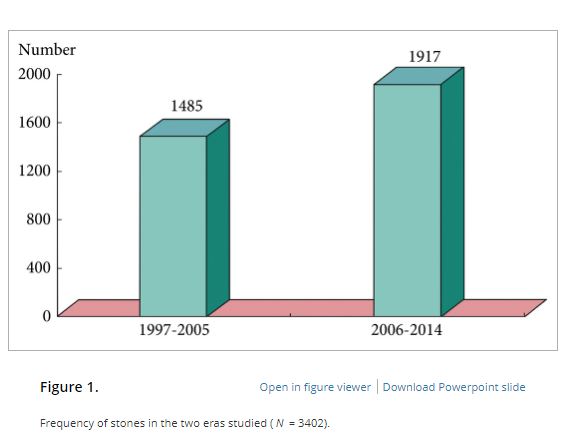
The follow up of small kidney stones is an uncertain area with very little written in either the EAU or AUA guidelines. Data from a meta-analysis by Ghani et al. shows that for every year of follow up on small kidney stones 7% may pass, 14% grow and 7% will require intervention. However, it is not possible in most health systems to follow everyone up forever and Mr Bultitude advocated increasing discharge rates from stone clinics to primary care after an agreed time of stability, allowing more on the complex and metabolic stone formers.Figure 1- Stone follow up algorithm
The expert stone panel then debated several challenging cases including “the encrusted stent”, stones in a pelvic kidney or calyceal diverticulum. These cases certainly are a challenge and require an individualized approach usually with multi-modality treatments.
Figure 2 – Stone expert panel
Upper tract urological biopsies are notoriously inaccurate, with only 15% of standard biopsies quantifiable histologically. Low grade tumours, are potentially suitable for endoscopic management with laser ablation. Dr Alberto Breda, from the urology department of Fundacio Puigvert Hospital in Spain, presented a novel solution for the future. This promising new technology uses confocal endomicroscopy to grade upper tract urological cancer. Initial results show 90% accuracy in diagnosing low grade tumours, which could then be safely managed endoscopically avoiding nephron-ureterectomy for some patients.
Figure 3 – Confocal endomicroscopy for upper tract malignancy
In the final session, a debate on BPH treatment, the audience preferred the bipolar resection technique for treating “the 60 year old with retention, with a 90 gram prostate and on rivaroxaban”, although HOLEP came a close second, with that talk giving the quote of the day “I spend more time with the morcellator than the wife.”
Figure 4 – Bipolar TURP wins the day
Nishant Bedi
ST4 Specialist urology registrar
Video: Comparing FG, USG and CG for renal access in mini-PCNL
A prospective and randomised trial comparing fluoroscopic, total ultrasonographic, and combined guidance for renal access in mini-percutaneous nephrolithotomy
Abstract
Objective
To compare the safety and efficacy of fluoroscopic guidance (FG), total ultrasonographic guidance (USG), and combined ultrasonographic and fluoroscopic guidance (CG) for percutaneous renal access in mini-percutaneous nephrolithotomy (mini-PCNL).
Patients and methods
The present study was conducted between July 2014 and May 2015 as a prospective randomised trial at the First Affiliated Hospital of Guangzhou Medical University. In all, 450 consecutive patients with renal stones of >2 cm were randomised to undergo FG, USG, or CG mini-PCNL (150 patients for each group). The primary endpoints were the stone-free rate (SFR) and blood loss (haemoglobin decrease during the operation and transfusion rate). Secondary endpoints included access failure rate, operating time, and complications. S.T.O.N.E. score was used to document the complexity of the renal stones. The study was registered at https://clinicaltrials.gov/ (NCT02266381).
Results
The three groups had similar baseline characteristics. With S.T.O.N.E. scores of 5–6 or 9–13, the SFRs were comparable between the three groups. For S.T.O.N.E. scores of 7–8, FG and CG achieved significantly better SFRs than USG (one-session SFR 85.1% vs 88.5% vs 66.7%, P = 0.006; overall SFR at 3 months postoperatively 89.4% vs 90.2% vs 69.8%, P = 0.002). Multiple-tracts mini-PCNL was used more frequently in the FG and CG groups than in the USG group (20.7% vs 17.1% vs 9.5%, P = 0.028). The mean total radiation exposure time was significantly greater for FG than for CG (47.5 vs 17.9 s, P < 0.001). The USG had zero radiation exposure. There was no significant difference in the haemoglobin decrease, transfusion rate, access failure rate, operating time, nephrostomy drainage time, and hospital stay among the groups. The overall operative complication rates using the Clavien–Dindo grading system were similar between the groups.
Conclusions
Mini-PCNL under USG is as safe and effective as FG or CG in the treatment of simple kidney stones (S.T.O.N.E. scores 5–6) but with no radiation exposure. FG or CG is more effective for patients with S.T.O.N.E. scores of 7–8, where multiple percutaneous tracts may be necessary.
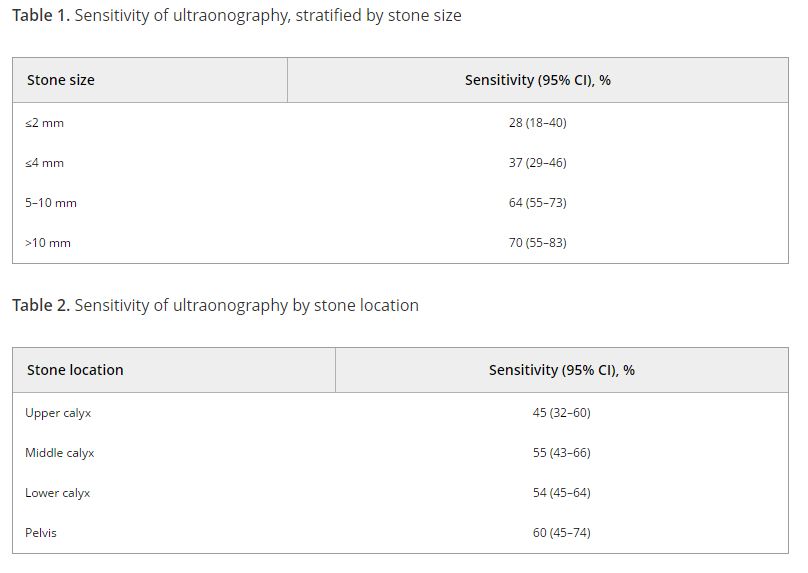
Article of the Week: Accuracy of ultrasonography for renal stone detection and size determination: is it good enough for management decisions?
Every week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video discussing the paper.
If you only have time to read one article this week, it should be this one.
Accuracy of ultrasonography for renal stone detection and size determination: is it good enough for management decisions?
*,†, *, *, * and *
*Glickman Urological Kidney Institute, and †Lerner College of Medicine, Cleveland Clinic, Cleveland, OH, USA
Abstract
Objectives
To determine the sensitivity and specificity of ultrasonography (US) for detecting renal calculi and to assess the accuracy of US for determining the size of calculi and how this can affect counselling decisions.
Materials and Methods
We retrospectively identified all patients at our institution with a diagnosis of nephrolithiasis who underwent US followed by non-contrast computed tomography (CT) within 60 days. Data on patient characteristics, stone size (maximum axial diameter) and stone location were collected. The sensitivity, specificity and size accuracy of US was determined using CT as the standard.
Results
A total of 552 US and CT examinations met the inclusion criteria. Overall, the sensitivity and specificity of US was 54 and 91%, respectively. There was a significant association between sensitivity of US and stone size (P < 0.001), but not with stone location (P = 0.58). US significantly overestimated the size of stones in the 0–10 mm range (P < 0.001). Assuming patients with stones 0–4 mm in size will be selected for observation and those with stones ≥5 mm could be counselled on the alternative of intervention, we found that in 14% (54/384) of cases where CT would suggest observation, US would lead to a recommendation for intervention. By contrast, when CT results would suggest intervention as management, US would suggest observation in 39% (65/168) of cases. An average of 22% (119/552) of patients could be inappropriately counselled. Stones classified as 5–10 mm according to US had the highest probability (43% [41/96]) of having their management recommendation changed when CT was performed. The use of plain abdominal film of kidney, ureter and bladder and US increases sensitivity (78%), but 37% (13/35) of patients may still be counselled inappropriately to undergo observation.
Conclusions
Using US to guide clinical decision-making for residual or asymptomatic calculi is limited by low sensitivity and inability to size the stone accurately. As a result, one in five patients may be inappropriately counselled when using US alone.