Scrotum Ulcer Developed After Intraperitoneal Hyperthermic Chemotherapy with Mitomycin-C
We report a pacient with a scrotum ulcer developed after intraperitoneal hyperthermic chemotherapy with mitomycin-C. There is only one article in the literature describing two similar cases. Our group suggests that an image investigation should be considered on male patients prior to intraperitoneal chemotherapy, since a procedure complication might be dramatic to the patient.
Authors: Silva, Fabiana; Avancini, Joao; Criado, Paulo; Pfiffer, Tulio; Lobo, Alice; Sanches, Jose
Corresponding Author: Silva, Fabiana
Case Report
A 65 year‐old Caucasian male patient with metastatic colorectal cancer was referred to the Dermatology Service with a scrotal ulcer in August 2011. The patient was diagnosed with rectal adenocarcinoma in 2008 and underwent rectosigmoidectomy with colostomy, followed by adjuvant radiotherapy and chemotherapy until May 2009. In February 2011 the patient was diagnosed with peritoneal tumor recurrence and in May 2011 he underwent a salvage surgical procedure with peritonectomy, hepatic metastasis excision and intraperitoneal hyperthermic chemotherapy with mitomycin‐C.
Nine days after this last procedure, the patient complained of scrotal pain and pruritus and slowly developed local erythema and edema that further evolved to a local ulceration. At first it was interpreted as local infection and the patient received systemic antibiotics including Cefalexin, and later Ciprofloxacin and Clindamycin without improvement.
In August 2011 the patient was referred to our Dermatology Department, presenting with scrotal induration and ulcer with dark eschars on the anterior wall of the scrotum, without evidence of scrotal abscess or Fournier’s gangrene (Figure 1).
A testicular ultrasound scan was performed, demonstrating signs of an inflammatory process of the scrotum, without testicular involvement. A cutaneous punch biopsy was performed and the histopathology was suggestive of ischemic necrosis, without positive findings on special histological stains for fungal and mycobacterial agents.
Tests for acquired and congenital thrombophilia were performed and no abnormalities were found. On September 2011 the patient underwent excision of the affected scrotal tissue that left the testicles exposed. The intraoperative findings were extensive deep necrosis with tunica albuginea involvement and thrombosis of local vasculature. Suture of the tunica vaginalis was performed protecting the testicles and vacuum assisted wound closure was used. The patient’s pain was relieved, and after one week he underwent another wound debridement and the scrotum was primarily repaired. There was suture dehiscence and a local dressing with Papain 8% was used with good response.
Discussion
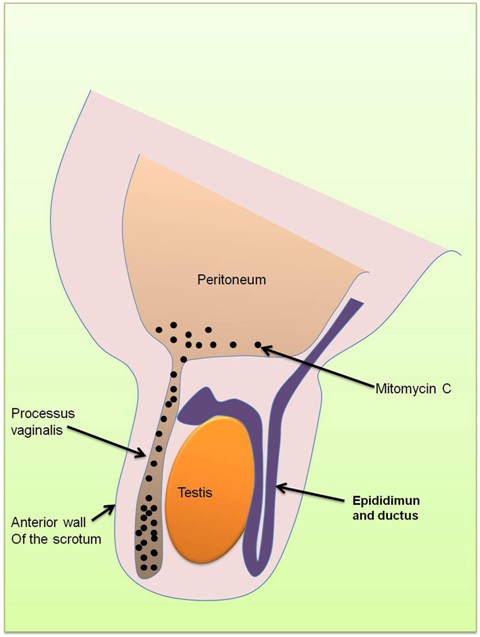
Akhavan A. et al (1) described two similar cases, and to our knowledge, our case is the third clinical report of a scrotal ulcer developing after intraperitoneal hyperthermic chemotherapy with mitomycin‐C. Two possible causes of the scrotal ulcers were proposed: (i) a patent processus vaginalis, allowing mitomycin‐C to become sequestered in the scrotum, inducing an inflammatory reaction, resulting in scrotal wall inflammation and subsequent ulceration (Figure 2). This was proposed since previous studies have shown that intradermal administration of mitomycin‐C inhibits wound healing and induces skin necrosis (2); (ii) local spillage of mitomycin‐C onto the scrotal skin, with resulting inflammation and ulceration.
Previous studies with patients on continuous ambulatory peritoneal dialysis (CAPD) have shown that 10% of CAPD patients developed genital swelling (3). A possible cause of the scrotal swelling is a patent processus vaginalis causing a communicating hydrocele, that can be found in 15–37% of adult men and may not be clinically evident until CAPD has begun (3, 4, 5, 6). Our group suggests that an image investigation, such as computed tomographic peritoneography (7), should be considered on male patients prior to intraperitoneal chemotherapy, since this complication is potentially serious for the patient.
Figure 1
Figure 2
References
1. Akhavan A, Yin M, Benoit R. Scrotal Ulcer After Intraperitoneal Hyperthermic Chemotherapy. UROLOGY. 2007; 69: p. 778.e9–778.e10.
2. Porter GT, Gadre SA, Calhoun KH. The effects of intradermal and topical mitomycin C on wound healing. Otolaryngol Head Neck Surg. 2006; 135: p. 56 – 60.
3.Kopecky RT, Funk MM, Kreitzer PR. Localised genital edema in patients undergoing continuous ambulatory peritoneal dialysis. 1985; 134: p. 880‐4.
4. Cochran ST, Do HM, Ronaghi A, Nissenson AR, Kadell BM. Complications of peritoneal dialysis: Evaluation with CT peritoneography. Radiographics. 1997; 17: p. 869‐78.
5. Litherland J, Gibson M, Sambrook P, Lupton E, Beaman M, Ackrill P. Investigation and treatment of poor drains of dialysate fluid associated with anterior abdominal wall leaks in patients on chronic ambulatory peritoneal dialysis. Nephrol Dial Transplant. 1992; 7: p. 1030‐4.
6. Hollett MD, Marn CS, Ellis JH, Francis IR, Swartz RD. Complications of continuous ambulatory peritoneal dialysis: Evaluation with CT peritoneography. AJR. 1992; 159: p. 983‐9.
7.Xie JY, Chen N, Shi T, Xu ZP, Lu Y, Ren H. Computed tomographic peritoneography in investigation of patent processus vaginalis in CAPD patients. Clin Nephrol. 2010; 73(2): p. 153‐6.
Date added to bjui.org: 21/10/2012
DOI: 10.1002/BJUIw-2012-019-web