Posts
Article of the week: Critical analysis of a multicentric experience with holmium laser enucleation of the prostate for BPH
Every week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
There is also an editorial written by a prominent member of the urological community. Please use the comment buttons if you would like to join the conversation.
If you only have time to read one article this week, we recommend this one.
Critical analysis of a multicentric experience with holmium laser enucleation of the prostate for benign prostatic hyperplasia: outcomes and complications of 10 years of routine clinical practice
Javier Romero-Otero*†‡, Borja García-Gómez*†, Lucía García-González*‡, Esther García-Rojo*, Pablo Abad-López*, Juan Justo-Quintas†, José Duarte-Ojeda*‡ and Alfredo Rodríguez-Antolín*
*Urology Department, Grupo de Investigación Salud Integral del Varón imas12, Hospital Universitario 12 Octubre, †Hospital Universitario HM Montepríncipe, and ‡Hospital Universitario La Luz, Madrid, Spain
Abstract
Objective
To assess the perioperative outcomes of holmium laser enucleation of the prostate (HoLEP) in real‐life practice and investigate the factors influencing the safety and effectiveness of the technique.
Patients and Methods
Critical analysis of patients with benign prostate hyperplasia (BPH) treated with HoLEP over 10 years of routine practice in three hospitals. Analysed variables included: preoperative characteristics (prostate size, active antiplatelet/anticoagulant therapy, blood parameters. prostate‐specific antigen (PSA) level, maximum urinary flow rate [Qmax], and International Prostate Symptom Score [IPSS]), intraoperative variables (operation time, concomitant removal of bladder calculi, and complications), early postoperative outcomes (change in blood parameters, catheterisation time, and hospital stay), and 12‐month follow‐up outcomes (change in IPSS, PSA level, and Qmax).
Results
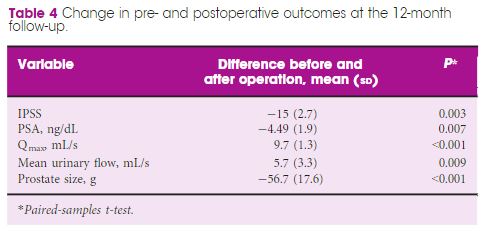
The analysis included 963 patients, aged 48–91 years, with a mean (range) prostate size of 91 (35–247) mL. The mean (sd ) operation time was 77 (29) min, and the hospital stay and catheterisation time were 4 (2) and 1.3 (2) days, respectively. In all, 56 patients (5.6%) required concomitant removal of bladder calculi and 36 (3.7%) were converted to open prostatectomy or transurethral resection of the prostate due to intraoperative complications. Patients had a significant decrease in haemoglobin and haematocrit, but no differences were seen between patients with and without anticoagulant/antiplatelet therapy and those with prostates ≥ and <100 mL. The concomitant removal of bladder calculi and having a prostate ≥100 mL resulted in a longer operation time, but did not influence the safety and effectiveness outcomes.
Conclusions
HoLEP is suitable for real‐life patients with BPH, irrespective of the presence of active treatment with anticoagulant/antiplatelet, bladder lithiasis or a prostate ≥100 mL.
Editorial: HoLEP is the complete technique for treating BPH
Ten years of experience with holmium laser enucleation of the prostate (HoLEP) are documented by Romero‐Otero et al. [1] and offer valuable insight into the real‐world use of this technique. No information on the 10‐year durability is available, however, as only the 12‐month data are presented, but there is a wealth of other information concerning both peri‐operative outcomes and complications. A particular strength of this paper is that all‐comers were studied, including patients with catheters, those with prostates larger than 100 g and those taking anti‐coagulants, plus there is the addition of the cases the three surgeons performed during their ‘learning curve’, although these are not analysed separately.
The authors’ technique almost certainly evolved over the study period. Personally, I currently find a one‐ or two‐piece enucleation to be more efficient than the three‐lobe technique originally described [2]. Enucleation efficiency of 1–2 g/min, as was achieved in this series (73 g in 40 min), is a good benchmark for tissue removal for those new to the technique and is a good measure of surgical proficiency. Being less aggressive anteriorly seems to have an impact on continence. It is often tempting to completely enucleate circumferentially in one continuous plane which is sometimes well beyond the commissure anteriorly. A more moderate dissection in this area can reduce the transient incontinence sometimes seen [3]. The incontinence rates in the current series of 12.8% at 3 months and 2.3% at 12 months are probably representative [1]. An analysis of the factors predisposing to moderate‐to‐severe incontinence in the six patients in this series would have been useful, particularly regarding prostate size, presence of a catheter and age.
The main contribution of HoLEP to the urological armamentarium is its ability to safely treat large prostates endoscopically [4]. Although robot‐assisted techniques have also decreased the morbidity of open prostatectomy [5], the attraction of the obvious ‘natural orifice’ for access and the use of laser technology for the enucleation with HoLEP is probably the least morbid and most cost‐effective way to treat these patients. Tackling a prostate larger than 100 g involves applying the same principles as for smaller prostates, with a few provisos. Firstly, having a consistent strategy for these large prostates is important and can be reassuring when things become difficult. Secondly, it is even more important to maintain the correct plane religiously as it is easier to get lost in these glands. A good sense of direction is important! Thirdly, stay ahead of the bleeding rather than trying to catch up as it can further compound an already difficult situation. Patience is a virtue.
The learning curve of HoLEP has historically been regarded as a major barrier to the uptake of the technique [6]. This has, of course, been exaggerated by proponents of other techniques, but it is important to emphasize that during this learning phase the excellent outcomes are maintained and that conversion to TURP, if necessary (3.4% in this series), can be safely done, as these authors’ have demonstrated. The length of the learning curve has been variously described as being between 20 and 80 cases and is almost entirely due to the way training is done. A modular mentored approach appears to be the best method and could equally be applied to endoscopic enucleation using any of the other energy sources that have been described [7].
HoLEP and all its progeny are here to stay, but which of these enucleation energy sources will gain ascendancy remains to be seen. Sadly, this will likely be more to do with the depth of the corporate pockets and their commitment to the cause rather than proper scientific appraisal [8].
by Peter Gilling
References
- Romero‐Otero J, Garcia‐Gomez B, Garcia‐Gonzalez L et al. Critical analysis of a multicentric experience with holmium laser enucleation of the prostate for benign prostatic hyperplasia: outcomes and complications of 10 years of routine clinical practice. BJU Int 2020; 126: 177-182
- Gilling PJ, Kennett K, Das AK, Thompson D, Fraundorfer MR. Holmium laser enucleation of the prostate (HoLEP) combined with transurethral tissue morcellation: an update on the early clinical experience. J Endourol 1998; 12: 457– 9
- Tunc L, Yalcin S, Kaya E et al. The “Omega Sign”: a novel HoLEP technique that improves continence outcomes after enucleation. World J Urol 2020 https://doi.org/10.1007/s00345-020-03152-9
- Gilling PJ, Kennett KM, Fraundorfer MR. Holmium laser enucleation of the prostate for glands larger than 100 g: an endourologic alternative to open prostatectomy. J Endourol 2000; 14: 529– 31
- Mourmouris P, Keskin SM, Skolarikos A et al. A prospective comparative analysis of robot‐assisted vs open simple prostatectomy for benign prostatic hyperplasia. BJU Int 2019; 123: 313– 7
- Placer J, Gelabert‐Mas A, Vallmanya F et al. Holmium laser enucleation of prostate: outcome and complications of self‐taught learning curve. Urology 2009; 73: 1042– 8
- Kuronen‐Stewart C, Ahmed K, Aydin A et al. Holmium Laser Enucleation of the prostate: simulation based training curriculum and validation. Urology 2015; 86: 639– 46.
- Herrmann TR. Enucleation is enucleation is enucleation is enucleation. World J Urol 2016; 34: 1353– 5
USANZ 2018: Melbourne
G’day! The 71st annual USANZ Congress, was held in Melbourne and had the biggest attendance on record for the past 6 years. The Urological Nurse’s congress: ANZUNS ran concurrently, encouraging multi disciplinary learning. An excellent and varied educational programme was masterminded by Declan Murphy, Nathan Lawrentschuk and their organising committee. Melbourne provided a great backdrop and soon felt like home with a rich and busy central business district, cultural and sporting venues, the Yarra river flowing past the conference centre, edgy graffiti and hipster coffee shops, plus too many shops, bars and restaurants to visit.
The programme included a day of masterclasses on a range of subjects, including: urological imaging, advanced robotic surgery with a live case from USC, metastatic prostate cancer and penile prosthetics. These were well attended by trainees and consultants alike. The PCNL session (pictured) with Professor Webb was popular and he generously gave his expertise. The session was supported by industry and provided an opportunity to use the latest nephroscopes on porcine models and innovative aids to realistically practice different puncture techniques.
Two plenary sessions were held each morning covering the breadth and depth of urology and were well attended. Dr Sotelo is always a highlight; he presented, to an auditorium of collective gasps, a unique selection of ‘nightmare’ cases His cases gave insight in how intraoperative complications occur and how they can be avoided. Tips, such as zooming out to reassess in times of anatomical uncertainty during laparoscopy or robotic surgery have great impact when you witness the possible consequences. Tim O’Brien shared his priceless insights on performing IVC thrombectomy highlighting the need for preoperative planning, early control of the renal artery and consideration of pre-embolisation. His second plenary on retroperitoneal fibrosis provided clarity on the management of this rare condition highlighting the role of PET imaging and, as with complex upper tract surgery, the importance of a dedicated team.
Tony Costello’s captivating presentation covered several myths in robotic prostate surgery, plus the importance of knowing your own outcome figures and a future where robotics will be cost equivalent to laparoscopy. Future technology, progress in cancer genomics and biomarkers were also discussed in various sessions. One example of new technology was Aquablation of the prostate; Peter Gilling presented the WATER trial results suggesting non-inferiority to TURP. A welcome addition to the programme was Victoria Cullen (pictured), a psychologist and Intimacy Specialist who provides education, support and strategies for sexual rehabilitation. She described her typical consultation with men with sexual dysfunction and how to change worries about being ‘normal’ to focusing on what is important to the individual.
Joint plenary sessions with the AUA and EAU were a particular highlight. Prof Chris Chapple confirmed the need for robust, evidence guidelines which support clinical decision making; and in many cases can be used internationally. He suggested collaboration is crucial between us as colleagues and scientists working in the field of urology. Stone prevention and analysis of available evidence was described by Michael Lipkin; unfortunately stone formers are usually under-estimaters of their fluid intake so encouragement is always needed! Amy Krambeck presented evidence for concurrent use of anticoagulants and antiplatelets during BOO surgery and suggested there can be a false sense of security when stopping these medications as it isn’t always safe. She championed HoLEP as her method of BOO surgery and continues medications, although the evidence does show blood transfusion rate may be higher. She also uses a fluid warming device which has less bleeding and therefore improved surgical vision; importantly it is preferred by her theatres nurses! MRI of the prostate was covered by many different speakers, however Jochen Walz expertly discussed the limitations of MRI in particular relating negative predictive value (pictured). He eloquently explained the properties of cribiform Gleason 4 prostate cancer and how this variant contributed to the incidence of false negatives.
Moderated poster and presentation sessions showcased research and audit projects from the UK, Australia, New Zealand and beyond, mainly led by junior urologists. The best abstracts submitted by USANZ trainees were invited to present for consideration of Villis Marshall and Keith Kirkland prizes. These prestigious prizes were valiantly fought for and reflected high quality research completed by the trainees. Projects included urethral length and continence, no need for lead glasses, obesity and prostate cancer, multi-centre management of ureteric calculi, mental health of surgical trainees and seminal fluid biomarkers in prostate cancer. This enthusiasm for academia will undoubtedly stand urology in good stead for the future; this line up (pictured) is one to watch!
The Trade hall provided a great networking space to be able to meet with friends and colleagues and engage with industry. It also hosted poster presentation sessions, with a one minute allocation for each presenter – which really ensures a succinct summary of the important findings (pictured)! It was nice to meet with Australian trainees and we discussed the highs and lows of training and ideas for fellowships. Issues such as clinical burden and operative time, selection into the specialty, cost of training, burn out and exam fears were discussed and shared universally; however there is such enthusiasm, a passion for urology and inspirational trainers which help balance burdens that trainees face. Furthermore, USANZ ‘SET’ Trainees were invited to meet with the international faculty in a ‘hot seat’ style session which was an enviable opportunity to discuss careers and aspirations.
In addition to the Congress I was fortunate to be invited for a tour and roof-top ‘barbie’ at the Peter Mac Cancer centre; plus a visit to Adelaide with Rick (Catterwell, co-author) seeing his new hospital and tucking into an inaugural Aussie Brunch. Peter Mac and Royal Adelaide Hospital facilities indicated an extraordinary level of investment made by Federal and State providers; the Peter Mac in particular had impressive patient areas, radiotherapy suites and ethos of linking clinical and research. However beyond glossy exteriors Australian public sector clinicians voiced concerns regarding some issues similar to those we face in the NHS.
Despite the distance of travelling to Melbourne and the inevitable jet lag the world does feels an increasingly smaller place and the Urological world even more so. There is a neighbourly relationship between the UK, Australia and New Zealand as evidenced by many familiar faces at USANZ who have worked between these countries; better for the new experiences and teaching afforded to them by completing fellowships overseas. The Gala Dinner was a great chance to unwind, catch up with friends and celebrate successes in the impressive surrounding of Melbourne Town Hall (pictured); the infamous organ played particularly rousing rendition of Phantom of the Opera on arrival.
The enthusiasm to strive for improvement is similar both home and away and therefore collaboration both nationally and internationally is integral for the progress of urology. The opening address by USANZ President included the phrase ‘together we can do so much more’ and this theme of collaboration was apparent throughout the conference. The future is bright with initiatives led by enthusiastic trainee groups BURST and YURO to collect large volume, high quality data from multiple centres, such as MIMIC which was presented by Dr Todd Manning. Social media, telecommunications and innovative technology should be used to further the specialty, especially with research and in cases of rare diseases – such as RPF. Twitter is a tool that can be harnessed and was certainly used freely with the hashtag #USANZ18. Furthermore, utilisation of educational learning platforms such as BJUI knowledge and evidence based guidelines help to facilitate high quality Urological practice regardless of state or country.
So we’d like to extend a huge thank you to Declan, Nathan and the whole team, and congratulate them for a successful, educational and friendly conference; all connections made will I’m sure last a lifetime and enable us to do more together.
Sophie Rintoul-Hoad and Rick Catterwell
Royal Society of Medicine: Key issues in Endourology
The RSM section of Urology #RSMUrology hosted a day on the Key issues in Endourology on 20th October. This was the first meeting of the academic year under President Roland Morley. Sri Sriprisad put together a complete endourology day with key subject areas of “PCNL and stones”, “upper tract TCC” and “BPH and retention”. Speakers from India, America and Spain provided expert opinions from around the globe.
The day started with the evolution of stone and urological laparoscopic surgery. Showing an insight into the challenges with the initial introduction of laparoscopic urological surgery. In order to allow surgeons the chance to discuss their experiences and troubleshoot and develop surgical techniques the SLUG forum (southern laparoscopic urology group) was created, which is still running today in the annual AUA meeting.
PCNL techniques were the subject for several debate lectures. Access for PCNL tracts was debated by Dr Janak Desai, visiting from Samved Urology hospital in India, arguing for fluoroscopic puncture with over 10,000 cases to date! Jonathan Glass, from Guy’s and St. Thomas’ Hospital, spoke for the prone position for the majority of PCNL, but selecting the supine position in 5-10% of cases depending on the anatomy and stone position. Dr Desai also spoke on ultra-mini PCNL, which he advocates using to treat solitary kidney stones under 2 cm in preference to flexible ureteroscopy.
The future of ESWL was debated and the audience voted that it is still “alive and clicking” by a narrow margin. However, although up to 80% clearance rates are quoted for upper pole stones less than 2 cm, the problem is that results of treatment are varied and unpredictable, and real-life success rates are far inferior. The variation in results may in part be due to the fact that there are no formal training courses for specialist radiographers nor SAC requirements for specialist registrars. Professor Sam McClinton presented on clinical research in stone disease with results from the TISU trial on primary ESWL vs. ureteroscopy for ureteric stones due out next year. The results will be fascinating and may help to decide if ESWL has a future in the UK.
Professor Margaret Pearle, visiting from the University of Texas Southwestern Medical Centre, explained the importance of treating residual fragments. With data showing that 20 – 36% of >2 mm residual stones after ureteroscopy required repeat surgery within 1 year. In a thought provoking lecture, she presented data showing that ureteroscopy may not be as good as we think and when critically examined, true stone-free rates maybe no better than ESWL. Maybe miniaturised PCNL is the way forward after all?
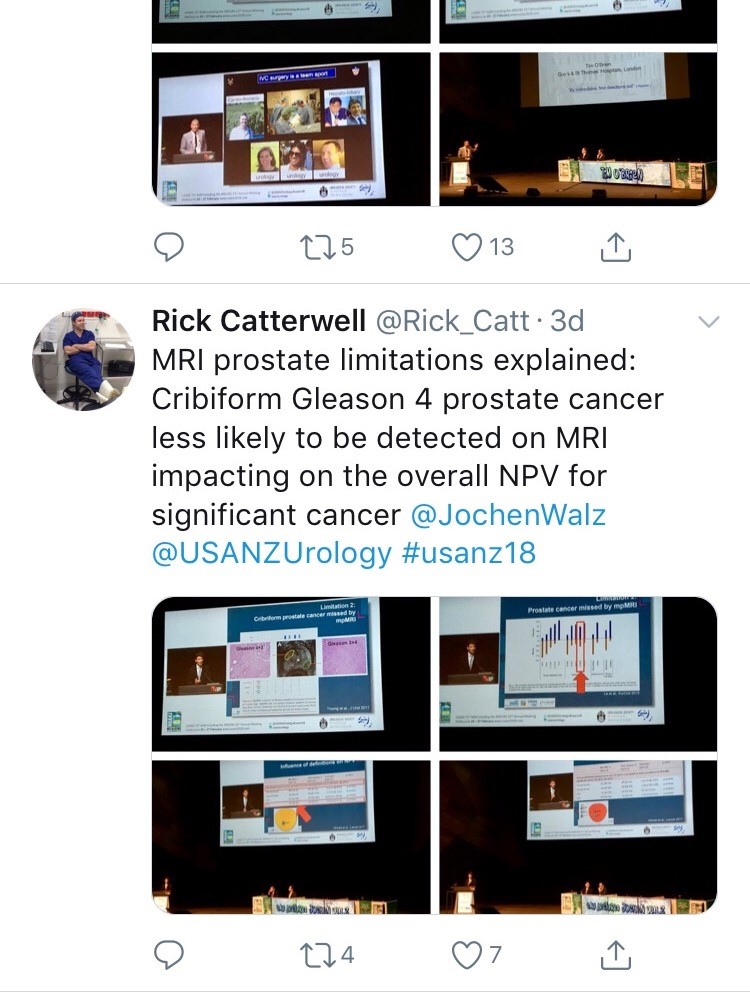
The follow up of small kidney stones is an uncertain area with very little written in either the EAU or AUA guidelines. Data from a meta-analysis by Ghani et al. shows that for every year of follow up on small kidney stones 7% may pass, 14% grow and 7% will require intervention. However, it is not possible in most health systems to follow everyone up forever and Mr Bultitude advocated increasing discharge rates from stone clinics to primary care after an agreed time of stability, allowing more on the complex and metabolic stone formers.Figure 1- Stone follow up algorithm
The expert stone panel then debated several challenging cases including “the encrusted stent”, stones in a pelvic kidney or calyceal diverticulum. These cases certainly are a challenge and require an individualized approach usually with multi-modality treatments.
Figure 2 – Stone expert panel
Upper tract urological biopsies are notoriously inaccurate, with only 15% of standard biopsies quantifiable histologically. Low grade tumours, are potentially suitable for endoscopic management with laser ablation. Dr Alberto Breda, from the urology department of Fundacio Puigvert Hospital in Spain, presented a novel solution for the future. This promising new technology uses confocal endomicroscopy to grade upper tract urological cancer. Initial results show 90% accuracy in diagnosing low grade tumours, which could then be safely managed endoscopically avoiding nephron-ureterectomy for some patients.
Figure 3 – Confocal endomicroscopy for upper tract malignancy
In the final session, a debate on BPH treatment, the audience preferred the bipolar resection technique for treating “the 60 year old with retention, with a 90 gram prostate and on rivaroxaban”, although HOLEP came a close second, with that talk giving the quote of the day “I spend more time with the morcellator than the wife.”
Figure 4 – Bipolar TURP wins the day
Nishant Bedi
ST4 Specialist urology registrar
RSM Urology Winter Meeting 2017, Northstar, California
This year’s Annual RSM Urology Section Winter Meeting, hosted by Roger Kirby and Matt Bultitude, was held in Lake Tahoe, California.
A pre-conference trip to sunny Los Angeles provided a warm-up to the meeting for a group of delegates who flew out early to visit Professor Indy Gill at the Keck School of Medicine. We were treated to a diverse range of live open, endourological and robotic surgery; highlights included a salvage RARP with extended lymph node dissection and a robotic simple prostatectomy which was presented as an alternative option for units with a robot but no/limited HoLEP expertise.
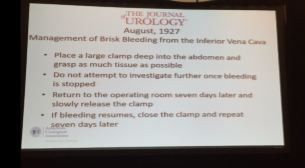
On arrival to Northstar, Dr Stacy Loeb (NYU) officially opened the meeting by reviewing the social media urology highlights from 2016. Next up was Professor Joseph Smith (Nashville) who gave us a fascinating insight into the last 100 years of urology as seen through the Journal of Urology. Much like today, prostate cancer and BPH were areas of significant interest although, in contrast, early papers focused heavily on venereal disease, TB and the development of cystoscopy. Perhaps most interesting was a slightly hair-raising description of the management of IVC bleeding from 1927; the operating surgeon was advised to clamp as much tissue as possible, close and then return to theatre a week later in the hopes the bleeding had ceased!
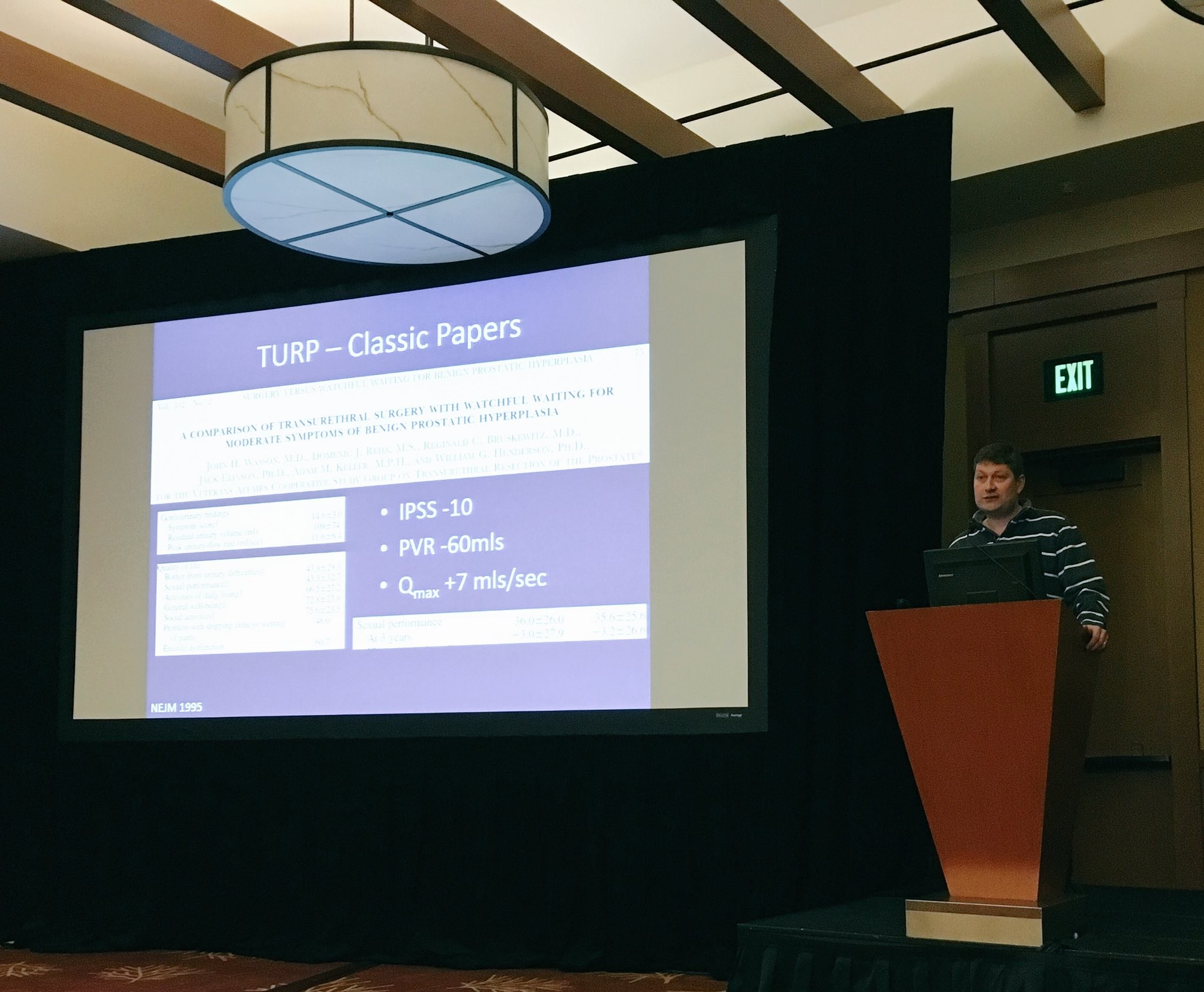
With the promise of beautifully groomed pistes and stunning views of Lake Tahoe, it was hardly surprising that the meeting was attended by a record number of trainees. One of the highlights of the trainee session was the hilarious balloon debate which saw participants trying to convince the audience of how best to manage BPH in the newly inaugurated President Trump. Although strong arguments were put forward for finasteride, sildenafil, Urolift, PVP and HoLEP, TURP ultimately won the debate. A disclaimer: this was a fictional scenario and, to the best of my knowledge, Donald Trump does not have BPH.
The meeting also provided updates on prostate, renal and bladder cancer. A standout highlight was Professor Nick James’ presentation on STAMPEDE which summarized the trial’s key results and gave us a taste of the upcoming data we can expect to see in the next few years.
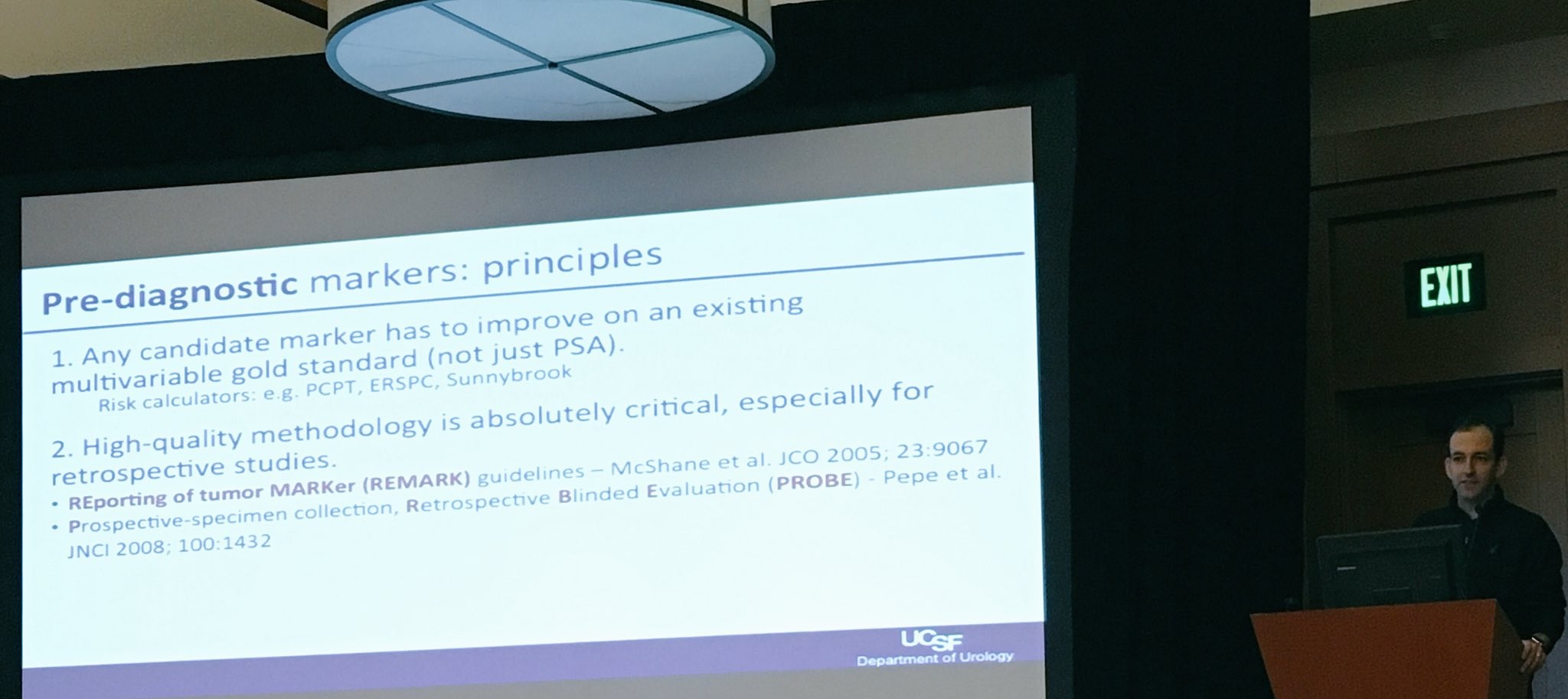
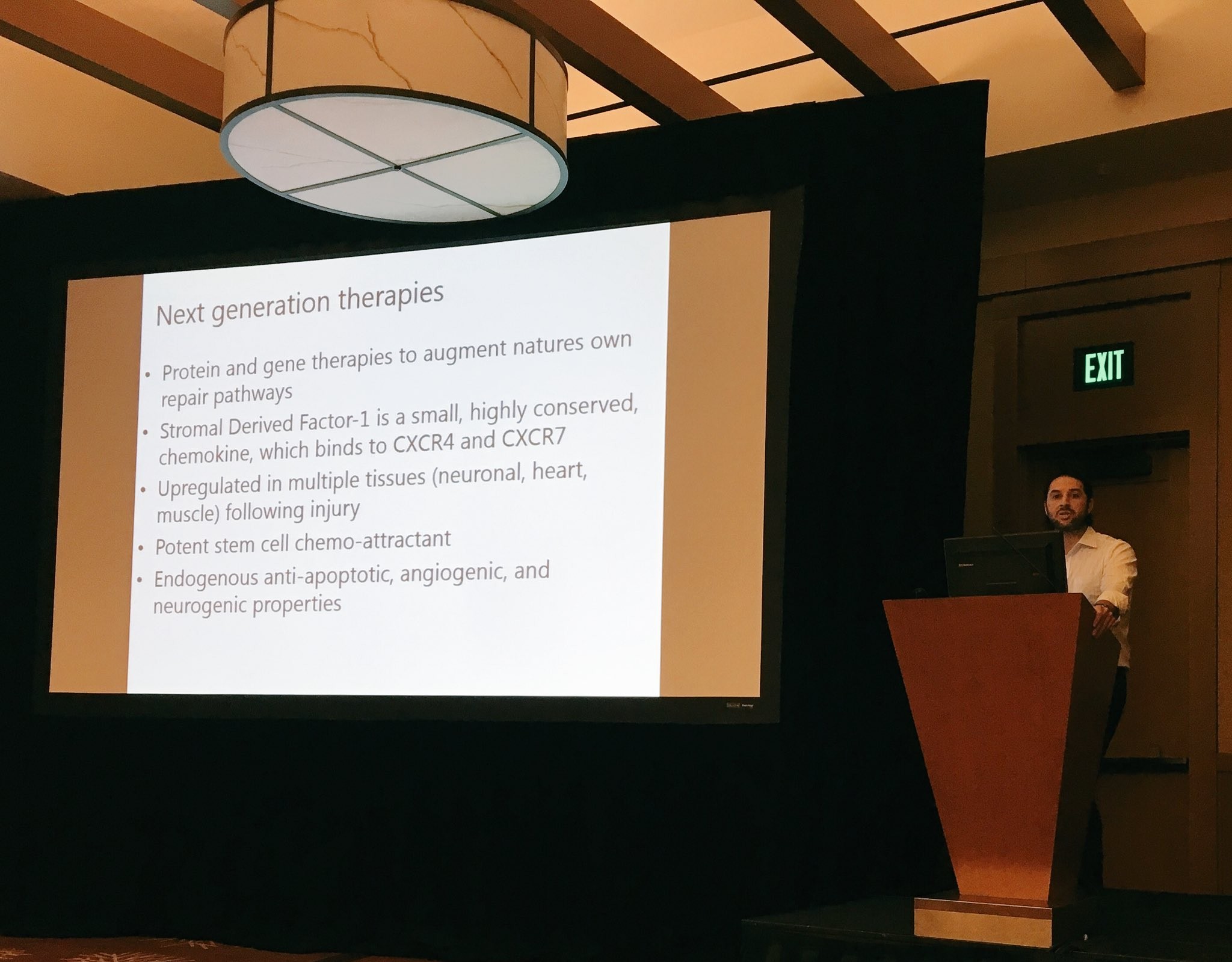
We were fortunate to be joined by prominent American faculty including Dr Trinity Bivalacqua (Johns Hopkins) and Dr Matt Cooperberg (UCSF) who provided state-of-the-art lectures on potential therapeutic targets and biomarkers in bladder and prostate cancer which promise to usher in a new era of personalized therapy.
A personal highlight was Tuesday’s session on learning from complications. It was great to hear some very senior and experienced surgeons speaking candidly about their worst complications. As a trainee, it served as a reminder that complications are inevitable in surgery and that it is not their absence which distinguishes a good surgeon but rather the ability to manage them well.
There was also plenty for those interested in benign disease, including topical discussions on how to best provide care to an increasingly ageing population with multiple co-morbidities. This was followed by some lively point-counterpoint sessions on robot-assisted versus open renal transplantation (Ravi Barod and Tim O’Brien), Urolift vs TURP (Tom McNicholas and Matt Bultitude) and HOLEP vs prostate artery embolization for BPH (Ben Challacombe and Rick Popert). Professor Culley Carson (University of North Carolina) concluded the session with a state-of-the art lecture on testosterone replacement.
In addition to the excellent academic programme, delegates enjoyed fantastic skiing with perfect weather and unparalleled views of the Sierra Nevada Mountains. For the more adventurous skiiers, there was also a trip to Squaw Valley, the home of the 1960 Winter Olympics. Another highlight was a Western-themed dinner on the shores of Lake Tahoe which culminated in almost all delegates trying their hand at line dancing to varying degrees of success! I have no doubt that next year’s meeting in Corvara, Italy will be equally successful and would especially encourage trainees to attend what promises to be another excellent week of skiing and urological education.
Miss Niyati Lobo
ST3 Urology Trainee, Brighton and Sussex University Hospitals NHS Trust
@niyatilobo