Have the days of ADT Monotherapy for Hormone Sensitive Prostate Cancer Come to an End? STAMPEDE in the June #urojc
The much awaited results of the STAMPEDE study of abiraterone for hormone naive prostate cancer was simultataneously presented at #ASCO17 and published ‘on line ahead of print’ in the NEJM. The formal title of the study was “Abiraterone for Prostate Cancer Not Previously Treated with Hormone Therapy”.
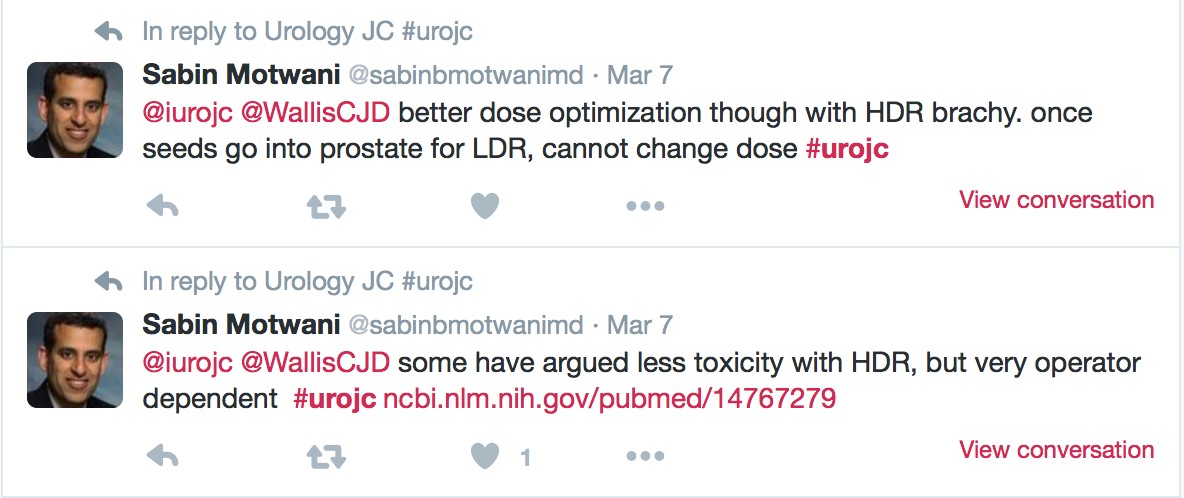
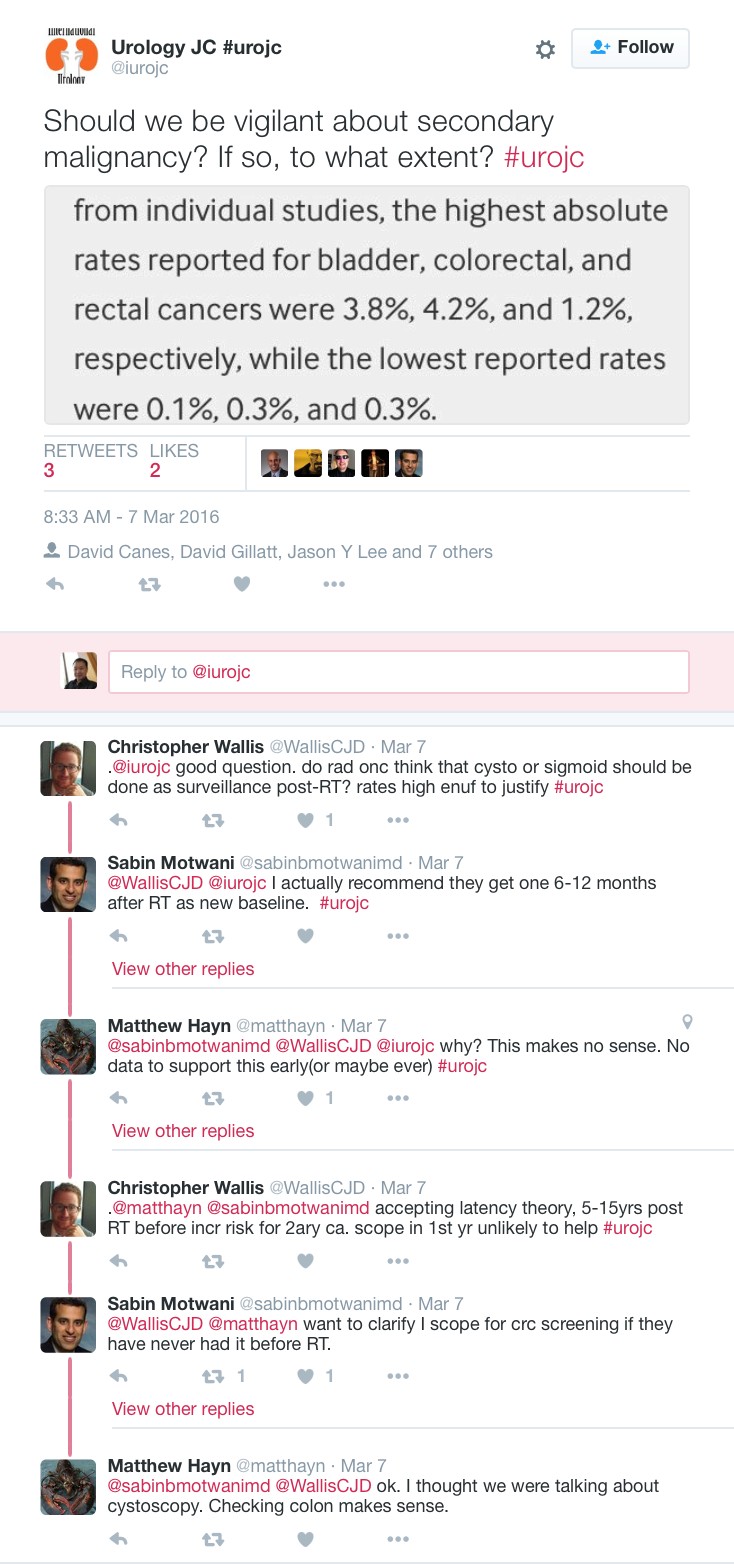
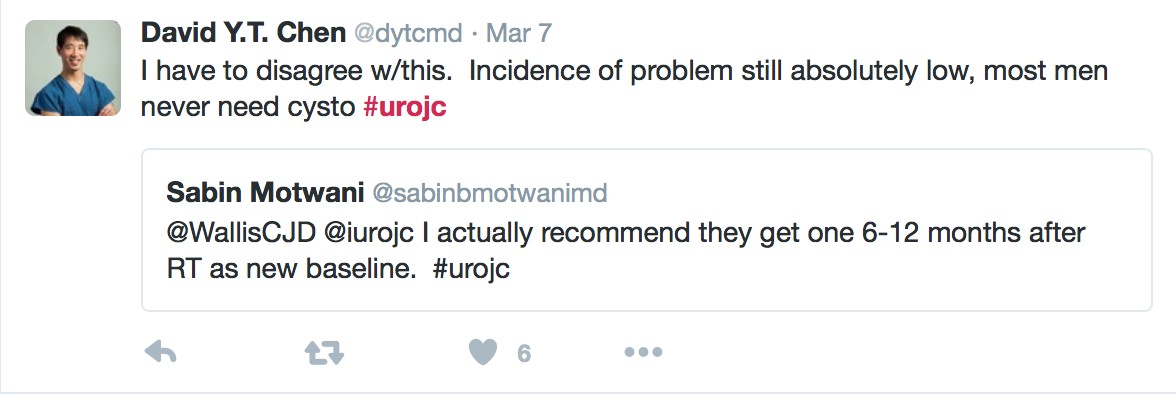
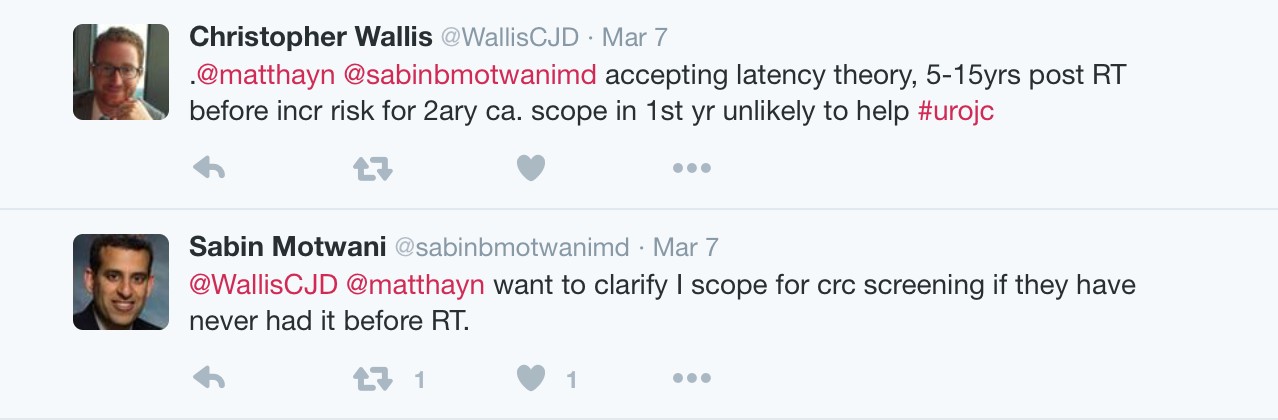
Briefly, the study randomised 1917 men with locally advanced or metastatic hormone naive prostate cancer to receive either ADT alone or ADT in combination with abiraterone and prednisolone. significantly higher rates of overall and failure-free survival than ADT alone.We were privileged to have the lead author Professor Nick James join us for the June #urojc. He posted the following video which is a lovely summary about STAMPEDE. All of us could benefit from watching this and it is a useful link for our patients.
— Nick James (@Prof_Nick_James) June 5, 2017
The data from the study is clear and it was not surprising that the majority of the discussion surrounding this paper was not going to be a dissection of the methodology or dataset and its analysis but rather how these results might impact upon urological practice.
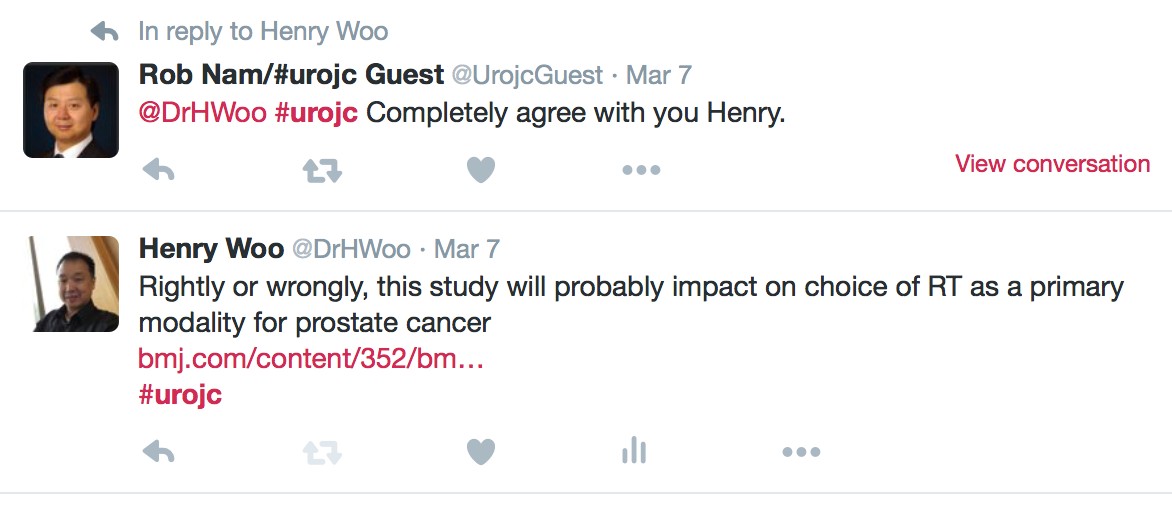
There was a somewhat provocative start to the discussion with:-
Are urologists prepared to prescribe abiraterone/prednisone?
Or do they wait & quietly hope that enza studies show as good efficacy?#urojc— Urology JC #urojc (@iurojc) June 4, 2017
Prepared and willing but will insurance pay for AA-P (in absence of CRPC)? #urojc— cp (@hosewater2) June 4, 2017
Need to monitor BP, LFTs etc makes prescribing AA impractical in urology clinic. Currently I leave it to Med Onc in chemoRx day ward— Garrett Durkan (@GCD67) June 4, 2017
#urojc Agreed, how could we not? But insurance coverage will be an issue in US until they accept STAMPEDE data.— Alan Hay (@alanhaymd) June 4, 2017
To turn the question around, we saw the following tweet:-
Why would we not prescribe abi? #urojc— Michael Douglas (@mddo5) June 4, 2017
Hmm….A couple of controversial excuses:-
1. Discomfort/lack of familiarity with prescribing Abi + P.
2. Obsession with robotics?#urojchttps://t.co/rlehsQDCzu— Henry Woo (@DrHWoo) June 4, 2017
But @urogeek came out swinging
I have been prescribing abi, enza and xofigo for years now. All are easier to give than BCG. Don’t understand why urologists are afraid— Dave Penson (@urogeek) June 4, 2017
Yes but it’s not hard to learn and it’s important urologists learn it. Believe me, learning robotics mid-career was a lot tougher— Dave Penson (@urogeek) June 5, 2017
But he was not alone in these thoughts.
In Germany those treatments are prescribed and monitored by urologist – works perfect @BertrandTOMBAL@urogeek@martin_schostak#ASC017— Axel Merseburger (@amerseburger) June 5, 2017
I agree with Dave, but it does take interest to learn the nuance. It would be like taking up robotics “just because” without real interest— David Morris (@DavidMorrismd) June 5, 2017
yes- we should use ABI-Both are great drugs for urologists to use but why wait! https://t.co/XnYX36VA3W— Judd Moul (@JuddMoul) June 4, 2017
But lets be fair, these responses are from urologists immersed in clinical trials experience and highly academic centers. The following tweet perhaps brought out what many were thinking.
With respect to Dr. Woo, it is a med outside our wheelhouse and @urogeek is uro onc trained. But that said, I’m going to have to learn it…— Michael Douglas (@mddo5) June 4, 2017
But perhaps the onus is upon us to make that extra effort to learn. As has been mentioned, we manage one of the most toxic agents competently in the form of intravesical BCG for bladder cancer.
That’s an important point & all the more important that urologists learn all about abiraterone https://t.co/ADvz4bHZrD#urojchttps://t.co/uaKP9mfhi3— Henry Woo (@DrHWoo) June 4, 2017
Naturally, there was bound to be some discussion about cost of treatment.
Not really news, but here’s the way to save $ on abi #urojchttps://t.co/X4TvfYS7r0— Nick Brook (@nickbrookMD) June 5, 2017
In the UK’s NHS, where abi is saved for castrate-resistant met prostate ca, can we afford the average of 33 months pts were on it? #urojc— Su-Min Lee (@leeurol) June 4, 2017
Typical duration 18m in CRPC and gain 3m OS. Duration 33m in HNPC so you buy 15m extra Abi and gain ~36 m OS. Probably cost effective— Nick James (@Prof_Nick_James) June 4, 2017
Magnitude of effect on OS probably similar and is cheaper! Q is would both be even better?— Nick James (@Prof_Nick_James) June 4, 2017
For a bit of light hearted banter, there was the following exchange which we hope nobody took too seriously.
— Urology JC #urojc (@iurojc) June 5, 2017
The twitter account of the journal Prostate Cancer and Prostatic Diseases posted a poll which was responded to by 117 participants with only 10% choosing the ADT alone option. Whilst far from scientific, does this represent a significant change in thinking? It was not long ago where we could have predicted that almost all respondents would have chosen the ADT alone option.
What would you now offer your hormone naive metastatic prostate putting aside cost/access/AE issues?#ASCO17#urojc— PCAN (@pcan_journal) June 3, 2017
And to finish up, a question answered by Nick James as follows:-
— Urology JC #urojc (@iurojc) June 5, 2017
A big thanks to all who participated in the June #urojc discussion. A special thanks to lead author Nick James for his insightful comments that really added to the discussion. We will be back for another installment of the #urojc in July. See you then.
Henry Woo (@drhwoo) is the Director of Uro-Oncology and Professor of Robotic Cancer Surgery at the Chris O’Brien Lifehouse in Sydney, Australia. He is also Professor Surgery at the Sydney Adventist Hospital Clinical School of the University of Sydney.















 JH population was "unique". Therapeutic benefit depends on the cohort being studied.
JH population was "unique". Therapeutic benefit depends on the cohort being studied. ) therapeutic benefit for standard PLND versus ePLND?
) therapeutic benefit for standard PLND versus ePLND?