Article of the month: Mortality after radical prostatectomy in a matched contemporary cohort in Sweden compared to the Scandinavian Prostate Cancer Group 4 study
Every month, the Editor-in-Chief selects an Article of the Month from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an editorial written by a prominent member of the urological community. These are intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Mortality after radical prostatectomy in a matched contemporary cohort in Sweden compared to the Scandinavian Prostate Cancer Group 4 (SPCG‐4) study
Abstract
Objectives
To investigate if results in terms of absolute risk in mature randomised trials are relevant for contemporary decision‐making. To do so, we compared the outcome for men in the radical prostatectomy (RP) arm of the Scandinavian Prostate Cancer Group Study number 4 (SPCG‐4) randomised trial with matched men treated in a contemporary era before and after compensation for the grade migration and grade inflation that have occurred since the 1980s.
Patients and Methods
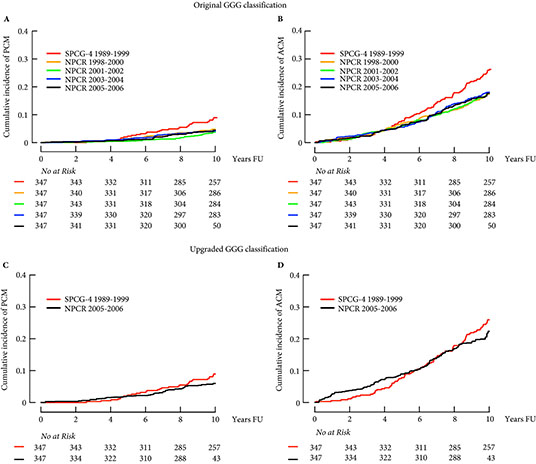
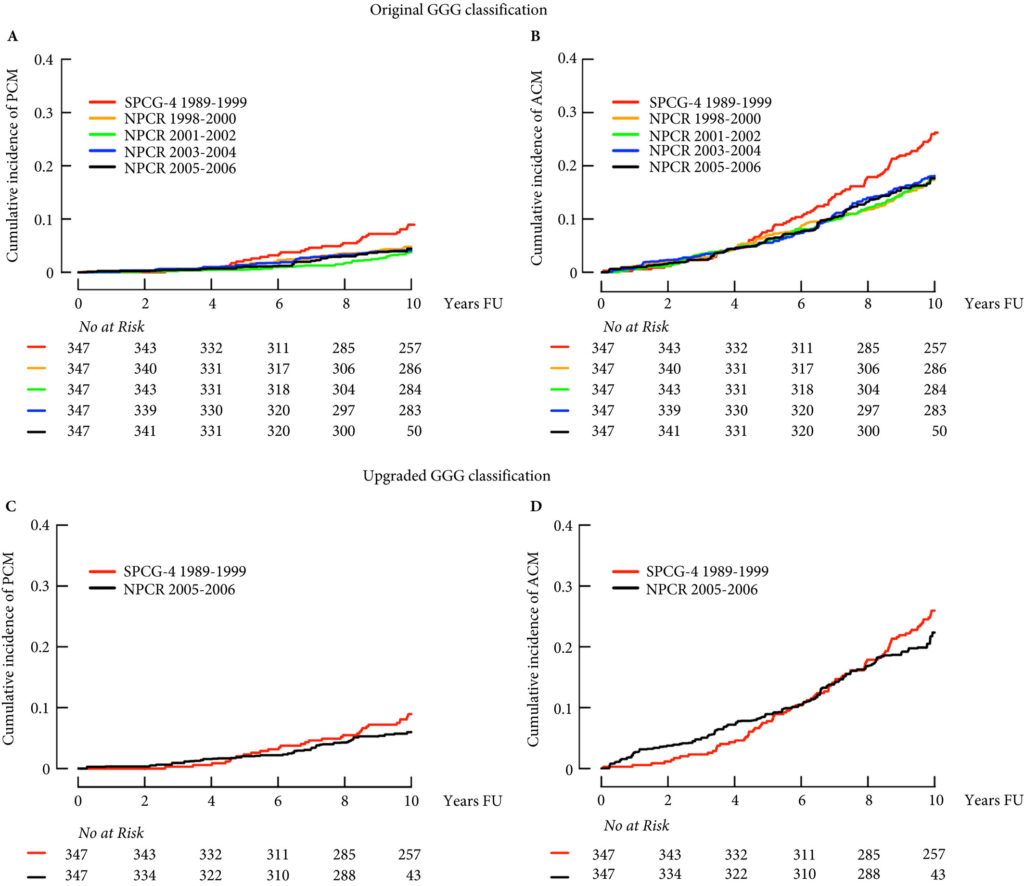
A propensity score‐matched analysis of prostate cancer mortality and all‐cause mortality in the SPCG‐4 and matched men in the National Prostate Cancer Register (NPCR) of Sweden treated in 1998–2006 was conducted. Cumulative incidence of prostate cancer mortality and all‐cause mortality was calculated. Cox proportional hazards regression analyses were used to estimate hazard ratios (HR) and 95% confidence intervals (CIs) for a matching on original Gleason Grade Groups (GGG) and second, matching with GGG increased one unit for men in the NPCR.
Results
Matched men in the NPCR treated in 2005–2006 had half the risk of prostate cancer mortality compared to men in the SPCG‐4 (HR 0.46, 95% CI 0.19–1.14). In analysis of men matched on an upgraded GGG in the NPCR, this difference was mitigated (HR 0.73, 95% CI 0.36–1.47).
Conclusion
Outcomes after RP for men in the SPCG‐4 cannot be directly applied to men in the current era, mainly due to grade inflation and grade migration. However, by compensating for changes in grading, similar outcomes after RP were seen in the SPCG‐4 and NPCR. In order to compare historical trials with current treatments, data on temporal changes in detection, diagnostics, and treatment have to be accounted for.