Article of the Week: Comparison of transperineal mpMRI/fusPbx and sysPbx
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Prospective comparison of transperineal magnetic resonance imaging/ultrasonography fusion biopsy and transrectal systematic biopsy in biopsy-naïve patients
Abstract
Objectives
To evaluate the value of multiparametric magnetic resonance imaging (mpMRI) in the detection of significant prostate cancer (PCa) and to compare transperineal MRI/ultrasonography fusion biopsy (fusPbx) with conventional transrectal systematic biopsy (sysPbx) in biopsy-naïve patients.
Patients and Methods
This multicentre, prospective trial investigated biopsy-naïve patients with suspicion of PCa undergoing transperineal fusPbx in combination with transrectal sysPbx (comPbx). The primary outcome was the detection of significant PCa, defined as Gleason pattern 4 or 5. We analysed the results after a study period of 2 years.
Results
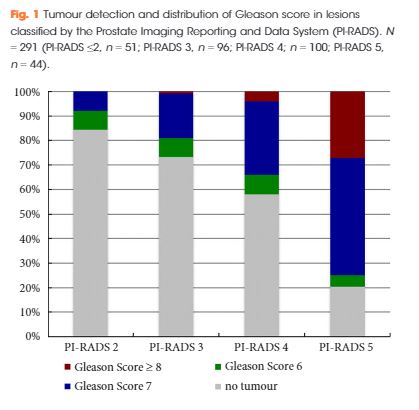
The study included 214 patients. The median (range) number of targeted and systematic cores was 6 (2–15) and 12 (6–18), respectively. The overall PCa detection rate of comPbx was 52%. FusPbx detected more PCa than sysPbx (47% vs 43%; P = 0.15). The detection rate of significant PCa was 38% for fusPbx and 35% for sysPbx (P = 0.296). The rate of missed significant PCa was 14% in fusPbx and 21% in sysPbx. ComPbx detected significantly more significant PCa than fusPbx and sysPbx alone (44% vs 38% vs 35%; P < 0.005). In patients presenting with Prostate Imaging Reporting and Data System (PI-RADS) 4 and 5 lesions there was a higher detection rate of significant PCa than in patients presenting with PI-RADS ≤3 lesions in comPbx (61% vs 14%; P < 0.005).
Conclusions
For biopsy-naïve men with tumour-suspicious lesions in mpMRI, the combined approach outperformed both fusPbx and sysPbx in the detection of overall PCa and significant PCa. Thus, biopsy-naïve patients may benefit from sysPbx in combination with mpMRI targeted fusPbx.