Article of the week: SEER shows no benefit from LND in RCC
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by prominent members of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Maxine Sun discussing her paper.
If you only have time to read one article this week, it should be this one
Extent of lymphadenectomy does not improve the survival of patients with renal cell carcinoma and nodal metastases: biases associated with the handling of missing data
Maxine Sun*, Quoc-Dien Trinh*‡, Marco Bianchi*¶, Jens Hansen*††, Firas Abdollah¶, Zhe Tian*, Shahrokh F. Shariat§, Francesco Montorsi¶, Paul Perrotte† and Pierre I. Karakiewicz*†
*Cancer Prognostics and Health Outcomes Unit, †Department of Urology, University of Montreal Health Center, Montreal, Canada, ‡Vattikuti Urology Institute, Henry Ford Health System, Detroit, MI, §Department of Urology,Weill Medical College of Cornell University, New York, NY, USA, ¶Department of Urology, Vita-Salute San Raffaele University, Milan, Italy, and ††Martini Clinic, Prostate Cancer Center Hamburg-Eppendorf, Hamburg, Germany
Maxine Sun and Quoc-Dien Trinh contributed equally to this study.
OBJECTIVE
• Previous studies showed no survival benefit with respect to performing lymph node dissection (LND) at nephrectomy, whereas a recent population-based analysis suggested otherwise, although the latter relied on imputation. To reconcile the findings of that study by critically evaluating the handling of missing data.
PATIENTS AND METHODS
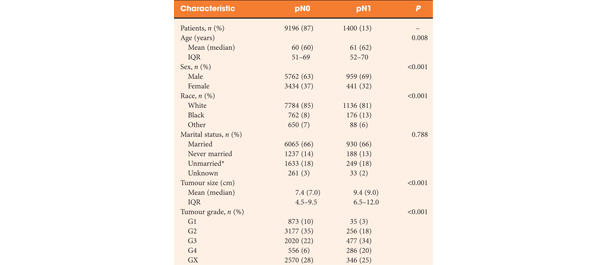
• Study participants comprised patients diagnosed with non-metastatic renal cell carcinoma (RCC) of all stages who underwent LND at nephrectomy (n = 10 596).
• Multivariable Cox regression models were performed to predict cancer-specific mortality (CSM), where the primary variable of interest was the extent of LND.
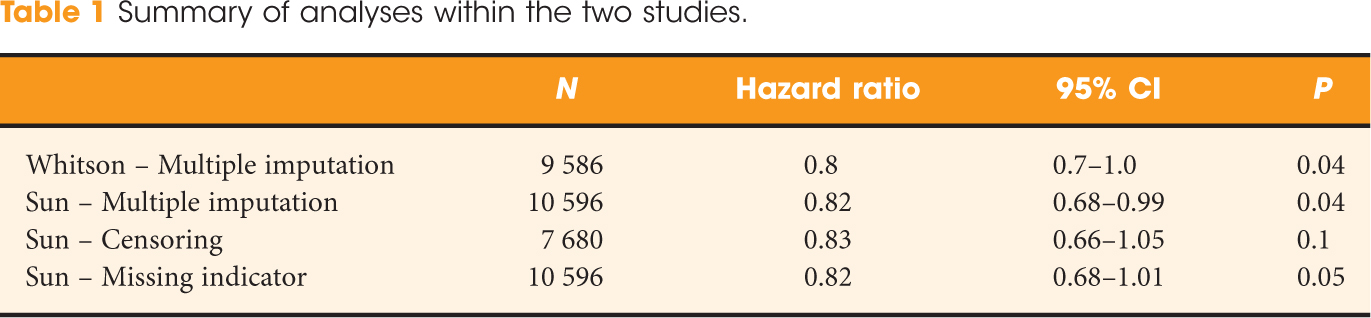
• To examine differences in approaches with respect to handling missing data, separate analyses were performed: (i) imputed population; (ii) exclusion of patients with missing data; and (iii) inclusion of patients with missing data as a sub-category.
RESULTS
• Overall, 2916 (28%) patients had missing tumour grade.
• In multivariable analyses, our findings showed that increasing the extent of LND was associated with a significant protective effect on CSM in patients with pN1 after imputation (hazard ratio [HR], 0.82; P = 0.04).
• By contrast, the extent of LND was no longer significantly associated with a lower risk of CSM after excluding patients with a missing tumour grade (HR, 0.83; P = 0.1) or when including patients with missing tumour grade as a sub-category (HR, 0.82; P = 0.05).
CONCLUSIONS
• The findings of the present study failed to corroborate the association of a survival benefit with increasing extent of LND at nephrectomy.
• The different methodologies employed to account for missing data may introduce important biases.
• Such considerations are non-negligible with respect to the interpretation of results for investigators who rely on administrative cohorts.
Read Previous Articles of the Week