Article of the week: Prostate biopsy: shaking up the old standard
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video of Dr Symons discussing his paper.
If you only have time to read one article this week, it should be this one.
Outcomes of transperineal template-guided prostate biopsy in 409 patients
James L. Symons*†, Andrew Huo*, Carlo L. Yuen‡§, Anne-Maree Haynes*, Jayne Matthews†, Robert L. Sutherland*, Phillip Brenner‡§ and Phillip D. Stricker†‡§
*Cancer Research Programme, Garvan Institute of Medical Research, †St Vincent’s Prostate Cancer Centre, ‡Department of Urology, St. Vincent’s Hospital, and §Department of Urology, St. Vincent’s Clinic, Darlinghurst, NSW, Australia
OBJECTIVE
• To present the template-guided transperineal prostate biopsy (TPB) outcomes for patients of two urologists from a single institution.
PATIENTS AND METHODS
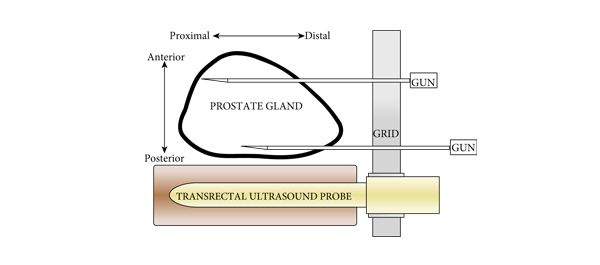
• We conducted a prospective study of 409 consecutive men who underwent TPB between December 2006 and June 2008 in a tertiary referral centre using a standardized 14-region technique.
• The procedure was performed as day surgery under general anaesthesia with fluoroquinolone antibiotic cover.
• Follow-up took place within 2 weeks, during which time men were interviewed using a standardized template.
• Results were compared with those of the Australian national prostate biopsy audits performed by the Urological Society of Australia and New Zealand (USANZ).
RESULTS
• Indications for biopsy included elevated prostate-specific antigen (PSA) level (75%), with a median PSA level of 6.5 ng/mL, abnormal digital rectal examination (8%) and active surveillance (AS) re-staging (18%).
• The mean patient age was 63 years and two-thirds of patients were undergoing their first biopsy.
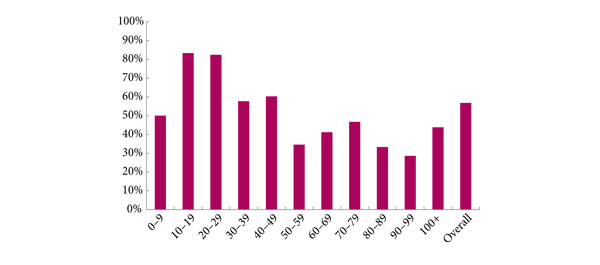
• A positive biopsy was found in 232 men, 74% of whom had a Gleason score of ≥7. The overall cancer detection rate was 56.7% (USANZ 2005 national audit = 56.5%). Stratified between those having their first TPB or a repeat procedure (after a previous negative biopsy), the detection rates were 64.4 and 35.6%, respectively. Significantly higher detection rates were found in prostates <50 mL in volume than in larger prostates (65.2 vs 38.3%, respectively, P < 0.001).
• Haematuria was the most common side effect (51.7%). Others included dysuria (16.4%), acute urinary retention (4.2%) and fever (3.2%). One patient (0.2%) had septicaemia requiring i.v. antibiotics.
• Repeat biopsy was not associated with increased complication rates.
CONCLUSIONS
• TPB is a safe and efficacious technique, with a cancer detection rate of 56.7% in the present series, and a low incidence of major side effects. Stratified by prostate volume, the detection rate of TPB was higher in smaller glands.
• Given the relatively low rate of serious complications, clinicians could consider increasing the number of TPB biopsy cores in larger prostates as a strategy to improve cancer detection within this group. Conversely, in patients on AS programmes, a staging TPB may be a superior approach for patients undergoing repeat biopsy so as to minimize their risk of serious infection.