Posts
Article of the Week: Retzius-sparing RALP: combining the best of retropubic and perineal approaches
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video demonstrating the Retzius-sparing approach to robot-assisted prostatectomy.
If you only have time to read one article this week, it should be this one.
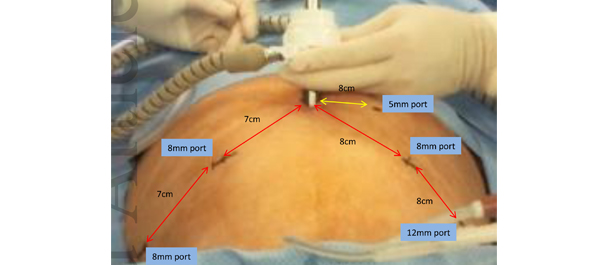
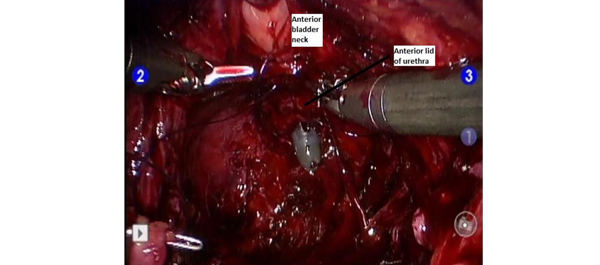
Retzius-sparing robot-assisted laparoscopic radical prostatectomy: combining the best of retropubic and perineal approaches
Sey Kiat Lim*†, Kwang Hyun Kim*, Tae-Young Shin*, Woong Kyu Han*, Byung Ha Chung*, Sung Joon Hong*, Young Deuk Choi* and Koon Ho Rha*
*Department of Urology, Urological Science Institute, Yonsei University College of Medicine, Seoul, South Korea and †Department of Urology, Changi General Hospital, Singapore
OBJECTIVE
To compare the early peri-operative, oncological and continence outcomes of Retzius-sparing robot-assisted laparoscopic radical prostatectomy (RALP) with those of conventional RALP.
MATERIALS AND METHODS
Data from 50 patients who underwent Retzius-sparing RALP and who had at least 6 months of follow-up were prospectively collected and compared with a database of patients who underwent conventional RALP. Propensity-score matching was performed using seven preoperative variables, and postoperative variables were compared between the groups.
RESULTS
A total of 581 patients who had undergone RALP were evaluated in the present study. Although preoperative characteristics were different before propensity-score matching, these differences were resolved after matching. There were no significant differences in mean length of hospital stay, estimated blood loss, intra- and postoperative complication rates, pathological stage of disease, Gleason scores, tumour volumes and positive surgical margins between the conventional RALP and Retzius-sparing RALP groups. Console time was shorter for Retzius-sparing RALP. Recovery of early continence (defined as 0 pads used) at 4 weeks after RALP was significantly better in the Retzius-sparing RALP group than in the conventional RALP group.
CONCLUSIONS
The present results suggest that Retzius-sparing RALP, although technically more demanding, was as feasible and effective as conventional RALP, and also led to a shorter operating time and faster recovery of early continence. Retzius-sparing RALP was also reproducible and achievable in all cases.
Editorial: Pushing the robot-assisted prostatectomy envelope – to the safety limits? Better outcomes
The present article by Lim et al. [1] describing the new technique for robot-assisted radical prostatectomy is provocative. It really does highlight the dramatic improvement in outcomes of prostate cancer surgery for men over the last 25 years. What used to be a 3-week hospital stay with a 50% incontinence rate and a 100% impotence rate [2, 3] now becomes a day case with a high likelihood of excellent urinary control early after surgery and a fair potential for potency preservation. Twenty-five years ago men who underwent radical prostatectomy were truly brave patients.
Lim et al. report a single series by the senior author of 50 cases performed using the so-called Retzius preservation technique. Their cohort of 50 patients treated this way was compared with a retrospective cohort of the surgeon’s patients. The patients had lower-risk disease and patients who had seminal vesicle invasion or extracapsular extension noted preoperatively, presumably on MRI, were excluded from the series. The authors report a shorter operating time and an earlier return to urinary continence in the first 6 months after surgery.
I guess where surgeons are now taking us is to an attempt to remove the prostate from the hammock of neurovascular, muscular and fascial tissue surrounding it, without disturbing the anatomy [4]. If this can be achieved then radical prostatectomy with minimal morbidity is a very compelling choice for the primary treatment of prostate cancer.
The authors’ hypothesis is that preservation of the levator fascia, puboprostatic ligaments and detrusor apron will fix the bladder somewhat like a sling would, with support at the bladder neck during increased intra-abdominal pressure.
It should be noted, however, that the present paper represents a single series of patients selected after a long learning curve by a very experienced surgeon. These excellent outcomes may simply reflect the fact that the surgeon is now extremely technically capable. It is contentious to assume that a propensity score matching of a retrospective cohort would represent a true comparator to contemporary outcomes. These excellent outcomes probably reflect technical improvements achievable with more risky and innovative surgery – after many cases. The authors should be congratulated on pushing the envelope to achieve even better outcomes for patients undergoing this operation, but the exclusion of patients with high-risk disease is probably the major negative aspect of their report. It has become increasingly obvious that patients with high-risk disease are those who benefit most from radical prostatectomy surgery. Surgery for patients with very-low-risk disease (Gleason 6) is probably unnecessary. Nevertheless, with continued insights such as those provided by these surgeons, we may be able to increase the range of patients to whom Retzius-sparing surgery in higher risk cohorts can be offered.
Anthony J. Costello
Department of Urology, Royal Melbourne Hospital, Parkville, Victoria, Australia
References
- Lim SK, Kim KH, Shin T-Y et al. Retzius-sparing Robot-assisted Laparoscopic Radical Prostatectomy – combining the best of retropubic and perineal approaches. BJU Int 2014; 114: 236–244
-
Wein AJ, Kavousi LR, Novick AC, Partin AW, Peters CA. Campbell-Walsh Urology, 10th edn. Saint Louis, MO: Saunders, 2011: 5688
-
Catalona WJ, Carvalhal GF, Mager DE, Smith DS. Potency, continence and complication rates in 1,870 consecutive radical retropubic prostatectomies. J Urol 1999; 162: 433–438
- Costello AJ, Brooks M, Cole OJ. Anatomical studies of the neurovascular bundle and cavernosal nerves. BJU Int 2004; 94: 1071–1076
Video: Retzius-sparing approach to RALP
Retzius-sparing robot-assisted laparoscopic radical prostatectomy: combining the best of retropubic and perineal approaches
Sey Kiat Lim*†, Kwang Hyun Kim*, Tae-Young Shin*, Woong Kyu Han*, Byung Ha Chung*, Sung Joon Hong*, Young Deuk Choi* and Koon Ho Rha*
*Department of Urology, Urological Science Institute, Yonsei University College of Medicine, Seoul, South Korea and †Department of Urology, Changi General Hospital, Singapore
OBJECTIVE
To compare the early peri-operative, oncological and continence outcomes of Retzius-sparing robot-assisted laparoscopic radical prostatectomy (RALP) with those of conventional RALP.
MATERIALS AND METHODS
Data from 50 patients who underwent Retzius-sparing RALP and who had at least 6 months of follow-up were prospectively collected and compared with a database of patients who underwent conventional RALP. Propensity-score matching was performed using seven preoperative variables, and postoperative variables were compared between the groups.
RESULTS
A total of 581 patients who had undergone RALP were evaluated in the present study. Although preoperative characteristics were different before propensity-score matching, these differences were resolved after matching. There were no significant differences in mean length of hospital stay, estimated blood loss, intra- and postoperative complication rates, pathological stage of disease, Gleason scores, tumour volumes and positive surgical margins between the conventional RALP and Retzius-sparing RALP groups. Console time was shorter for Retzius-sparing RALP. Recovery of early continence (defined as 0 pads used) at 4 weeks after RALP was significantly better in the Retzius-sparing RALP group than in the conventional RALP group.
CONCLUSIONS
The present results suggest that Retzius-sparing RALP, although technically more demanding, was as feasible and effective as conventional RALP, and also led to a shorter operating time and faster recovery of early continence. Retzius-sparing RALP was also reproducible and achievable in all cases.
Article of the week: Men under 50 should not be discouraged from radical prostatectomy
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by prominent members of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Dr. Andreas Becker discussing his paper.
If you only have time to read one article this week, it should be this one.
Functional and oncological outcomes of patients aged <50 years treated with radical prostatectomy for localised prostate cancer in a European population
Andreas Becker*†, Pierre Tennstedt*, Jens Hansen*, Quoc-Dien Trinh†, Luis Kluth‡, Nabil Atassi*, Thorsten Schlomm*, Georg Salomon*, Alexander Haese*, Lars Budaeus*, Uwe Michl*, Hans Heinzer*, Hartwig Huland*, Markus Graefen* and Thomas Steuber*
*Martini-Clinic, Prostate Cancer Center Hamburg-Eppendorf, Hamburg, Germany, †Cancer Prognostics and Health Outcomes Unit, University of Montreal Health Center, Montreal, Canada, and ‡Department of Urology, University-Hospital Hamburg-Eppendorf, Hamburg, Germany
OBJECTIVE
• To address the biochemical and functional outcomes after radical prostatectomy (RP) of men aged <50 years in a large European population.
PATIENTS AND METHODS
• Among 13 268 patients who underwent RP for clinically localised prostate cancer at our centre (1992–2011), 443 (3.3%) men aged <50 were identified.
• Biochemical recurrence (BCR) and functional outcomes (International Index of Erectile Function [IIEF-5], use of pads), were prospectively evaluated and compared between men aged <50 years and older patients.
RESULTS
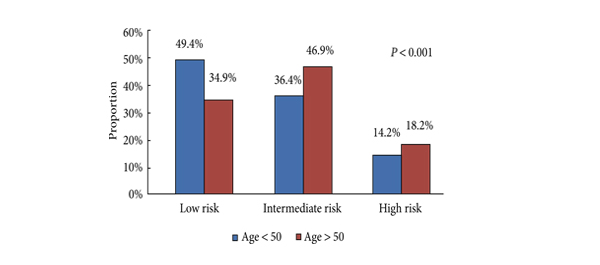
• Men aged <50 years were more likely to harbour D’Amico low-risk (49.4 vs 34.9%, P < 0.001), organ-confined (82.6 vs 69.4%, P < 0.001) and low-grade tumours (Gleason score <7: 33.1 vs 28.7%, P < 0.001).
• Multivariate Cox regression analysis showed that age <50 years (hazard ratio 0.99; confidence interval 0.72–1.31; P = 0.9) was not a predictor of BCR.
• Urinary continence was more favourable in younger patients, resulting in continence rates of 97.4% vs 91.6% in most recent years (2009–2011) for patients aged <50 vs ≥50 years.
• After RP, a median IIEF-5 drop of 4 points in younger men vs 8 points in older patients was recorded (P < 0.001).
• Favourable recovery of urinary continence and erectile function in patients aged <50 years compared with their older counterparts was confirmed after multivariable adjustment.
CONCLUSION
• Men aged <50 years diagnosed with localised prostate cancer should not be discouraged from RP, as the postoperative rates of urinary incontinence and erectile dysfunction are low and probability of BCR-free survival at 2 and 5 years is high.
Editorial: Radical prostatectomy at young age
Becker et al. [1] investigated a large sample of young patients (aged <50 years) who underwent radical prostatectomy during a 20-year period in a high-volume European centre. In this study [1], men aged <50 years had a significantly more favourable functional outcome (continence rates [0–1 pads] 97% vs 92%; International Index of Erectile Function [IIEF] score drop of 4 vs 8 points), compared with their older counterparts. Biochemical tumour control was higher in younger patients in univariate (5-year rates 81% vs 70%) but not in multivariate analysis.
In studies in the pre-PSA era, young age at prostate cancer diagnosis was often associated with adverse tumour-related outcome [2]. Possibly, the disadvantage of younger patients was attributable to rapidly growing high-grade tumours causing symptoms at a young age in the absence of a dilution by favourable early detected low-grade cancers. In contemporary patients, the opposite is observed [1]. As the impact of age vanished after controlling for tumour-related prognostic factors reflecting the presence of more favourable disease criteria in younger men, it may be considered likely that PSA-based early detection enriched favourable parameters in the younger subgroup. Altogether, prostate cancer biology is probably not meaningfully associated with age. Outcome differences, even in randomised trials [3, 4], are rather caused by age-related differences in the approach to prostate cancer diagnostics and early detection than in actual biological differences.
The relative favourable functional outcome in younger patients [1] supports early curative treatment in this population. Currently available active surveillance studies have very limited follow-up and were performed mainly in elderly patients with significant comorbidity [5]. Currently, in Germany the further life expectancy in men aged 50 years is ≈30 years [6]. In a contemporary active surveillance study, narrowly half of patients received active treatment within 10 years [5]. Therefore, most men starting active surveillance at an age of 50 years will subsequently receive active treatment. This treatment will then be performed at a greater age where the chances for satisfactory functional recovery are less favourable.
The inferior tumour control rates in patients receiving robot-assisted surgery is another remarkable finding of this study (hazard ratio 1.4, 95% CI 0.99–1.9, P = 0.06 in the multivariate analysis). Although the significance level was narrowly failed, this observation cannot be ignored. It was accompanied by an increased continence recovery rate after robot-assisted surgery suggesting that it may probably not be attributed to the learning curve. Less radical removal of the prostate with more sparing of neurovascular structures and bladder neck might be a conceivable explanation of this phenomenon. In this study [1], the prognostic impact of robot-assisted approach was in a similar range as a positive surgical margin (hazard ratio 1.5, 95% CI 1.4–1.7).
Current clinical guidelines discourage prostate cancer screening in average-risk men aged <50 years [7]. It remains to be seen in which degree these recommendations will affect clinical practice and outcome parameters in this age group in the years ahead.
Manfred P. Wirth and Michael Froehner
Department of Urology, University Hospital ‘Carl Gustav Carus’, Dresden University of Technology, Dresden, Germany
References
- Becker A, Tennstedt P, Hansen J et al. Functional and oncological outcomes of patients younger than 50 years treated with radical prostatectomy for localized prostate cancer in a European population. BJU Int 2014; 114: 38–45
- Parker CC, Gospodarowicz M, Warde P. Does age influence the behaviour of localized prostate cancer? BJU Int 2001; 87: 629–637
- Bill-Axelson A, Holmberg L, Ruutu M et al. Radical prostatectomy versus watchful waiting in early prostate cancer. N Engl J Med 2011; 364: 1708–1717
- Froehner M, Wirth MP. Early prostate cancer – treat or watch? N Engl J Med 2011; 365: 568
- Selvadurai ED, Singhera M, Thomas K et al. Medium-term outcomes of active surveillance for localised prostate cancer. Eur Urol 2013; 64: 981–987
- Statistisches Bundesamt. Periodensterbetafeln für Deutschland 1871/1881 bis 2008/2010 [Period death tables for Germany 1871/1881 bis 2008/2010]. Wiesbaden 2012. Available at: https://www.destatis.de/DE/Publikationen/Thematisch/Bevoelkerung/Bevoelkerungsbewegung/PeriodensterbetafelnPDF_5126202.pdf?__blob=publicationFile [Website in German]. Accessed 12 July 2013.
- Qaseem A, Barry MJ, Denberg TD, Owens DK, Shekelle P; Clinical Guidelines Committee of the American College of Physicians. Screening for prostate cancer: a guidance statement from the Clinical Guidelines Committee of the American College of Physicians. Ann Intern Med 2013; 158: 761–769
Video: RP for younger men – low risk and high survival rate
Functional and oncological outcomes of patients aged <50 years treated with radical prostatectomy for localised prostate cancer in a European population
Andreas Becker*†, Pierre Tennstedt*, Jens Hansen*, Quoc-Dien Trinh†, Luis Kluth‡, Nabil Atassi*, Thorsten Schlomm*, Georg Salomon*, Alexander Haese*, Lars Budaeus*, Uwe Michl*, Hans Heinzer*, Hartwig Huland*, Markus Graefen* and Thomas Steuber*
*Martini-Clinic, Prostate Cancer Center Hamburg-Eppendorf, Hamburg, Germany, †Cancer Prognostics and Health Outcomes Unit, University of Montreal Health Center, Montreal, Canada, and ‡Department of Urology, University-Hospital Hamburg-Eppendorf, Hamburg, Germany
OBJECTIVE
• To address the biochemical and functional outcomes after radical prostatectomy (RP) of men aged <50 years in a large European population.
PATIENTS AND METHODS
• Among 13 268 patients who underwent RP for clinically localised prostate cancer at our centre (1992–2011), 443 (3.3%) men aged <50 were identified.
• Biochemical recurrence (BCR) and functional outcomes (International Index of Erectile Function [IIEF-5], use of pads), were prospectively evaluated and compared between men aged <50 years and older patients.
RESULTS
• Men aged <50 years were more likely to harbour D’Amico low-risk (49.4 vs 34.9%, P < 0.001), organ-confined (82.6 vs 69.4%, P < 0.001) and low-grade tumours (Gleason score <7: 33.1 vs 28.7%, P < 0.001).
• Multivariate Cox regression analysis showed that age <50 years (hazard ratio 0.99; confidence interval 0.72–1.31; P = 0.9) was not a predictor of BCR.
• Urinary continence was more favourable in younger patients, resulting in continence rates of 97.4% vs 91.6% in most recent years (2009–2011) for patients aged <50 vs ≥50 years.
• After RP, a median IIEF-5 drop of 4 points in younger men vs 8 points in older patients was recorded (P < 0.001).
• Favourable recovery of urinary continence and erectile function in patients aged <50 years compared with their older counterparts was confirmed after multivariable adjustment.
CONCLUSION
• Men aged <50 years diagnosed with localised prostate cancer should not be discouraged from RP, as the postoperative rates of urinary incontinence and erectile dysfunction are low and probability of BCR-free survival at 2 and 5 years is high.
The indwelling Foley Catheter; an anachronism
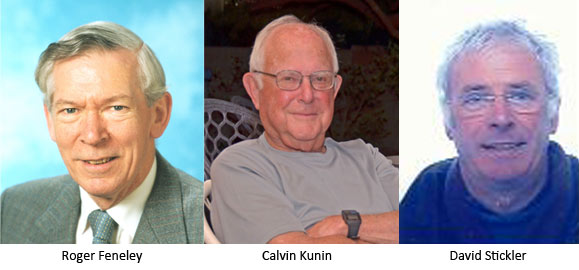
The Simon Foundation for Continence was founded in 1982 by Cheryle Gartley to bring the subject into the open, remove the stigma surrounding incontinence and provide help and hope to the individuals. their families and their healthcare professionals. As President, Cheryle invited Roger Feneley, Calvin Kunin and David Stickler to the Foundations’ third conference in the series entitled Innovating for Continence: The Engineering Challenge in 2011, to talk about catheter drainage of the bladder. Their presentations each carried the same message that the design of the indwelling Foley catheter violated the integrity of the sophisticated defence mechanisms that protect the bladder from bacterial infection. The morbidity and mortality caused by the Foley catheter and their costs to health services are no longer acceptable. Research and Development of antimicrobial coatings alone will not resolve the problems of long-term catheterisation.
This meeting led to their publication ‘An indwelling catheter for the 21st Century’ in the BJUI. In an era witnessing outstanding technological advances in medical implants the simple task of draining urine from the bladder should be performed without producing infection and a range of associated complications. The cyclical filling and emptying of the bladder is crucial to the bladder’s defence against bacterial infection but the design of the Foley catheter with the drainage eyes in its protruding tip distal to the self-retaining balloon not only prevents the bladder from emptying completely but can seriously damage the integrity of the protective urothelial lining. Medical device manufacturers need to take up the challenge of producing a device which restores the function of the debilitated lower urinary tract without threatening its health.
This video explains the problem further.
The Simon Foundation’s 4th international conference, Innovating for Continence: The Engineering Challenge takes place this week in Chicago, IL
Dr David Stickler became interested in the problem of catheter-associated urinary tract infections in paraplegic patients at the Irish National Spinal Unit during his time as a lecturer in Trinity College Dublin in the early 1970s. Over the years as a reader in medical microbiology in Cardiff University he worked on many aspects of the problem from the fundamental biology of the bacterial biofilms that develop on catheters to the practical management of biofilm-induced catheter encrustation and blockage. Currently he is an honorary senior research fellow in the Cardiff University School of Biosciences.
Dr. Kunin received his MD from Cornell University College of Medicine in 1953. He is Emeritus Professor of Medicine at the Ohio State University and Clinical Professor of Medicine at the University of Arizona. He has a distinguished background in infectious diseases, antimicrobial pharmacology, hospital infection control, urinary tract infections and promotion of appropriate use of antibiotics. He has published over 350 scientific articles and a book on urinary tract infections. He is a past president of the Infectious Diseases Society of American, served on NIH and FDA advisory committees and is an honorary academic consultant to the National Health Research Institute in Taiwan.
Mr Roger Feneley is an Emeritus Consultant Urologist to the North Bristol NHS Trust and Visiting Professor in the Faculty of Applied Science at the University of the West of England (UWE). In 1998 he founded the BioMed Centre within the Bristol Urological Institute with the objective to improve the care of patients with intractable urinary incontinence. In 2009, he founded Alternative Urological Catheter Systems Ltd to develop new urine collection systems.
Comments on this blog are now closed.