Air embolism is a rare unpredictable complication after CT guided tranthoracic needle biopsy of lung masses but potentially fatal if not managed correctly and urgently. We present a case of cerebral air embolism following lung nodule biopsy manifested by seizure and left hemiparesis. The patient had a full recovery following 100% oxygenotherapy.
Authors: Maalouly, Rina Antou ; Tannouri, Fadi; Mattar, Hanna; Kassis, Antoine
Corresponding Author: Maalouly, Rina Antoun
Introduction
Computed tomography guided percutaneous transthoracic needle biopsy (PTNB) of lung lesions isa well established diagnostic procedure for the evaluation of lung masses. It provides high diagnostic accuracy with excellent sensitivity and specificity (>90%) in the diagnosis of lung cancer, metastasis or benign lesions.
As for all interventional procedures, some complications may occur. The most frequent ones for PTNB are pneumothorax (27%), haemorrhage (11%) and haemoptysis (7%). A rare but not to miss fatal complication is systemic air embolus, occurring at a rate of 0.07%1.
We present a case of cerebral air embolism clinically manifested by complete disorientation, hemiparesis, convulsion and loss of consciousness in a 53 year old male just after a CT guided lung biopsy. The patient had a full recovery after 100% oxygentherapy.
Case report
A 53 year old male patient diagnosed with testicular cancer (Non SeminomatousGerminal Cell Tumor) surgically treated 4 years previous to presentation, was admitted for follow up. A chest CT scan (5mm thicknesscomputed tomography; Prospeed GE Medical System) showed a new, well-margined 0.8 cm nodule at the apex of the left lower lobe. Findings were suggestive of a secondary lesion and a CT guided biopsy was requested for diagnosis as both testicular tumourmarkers, α-foetoprotein and βHCG, were negative.
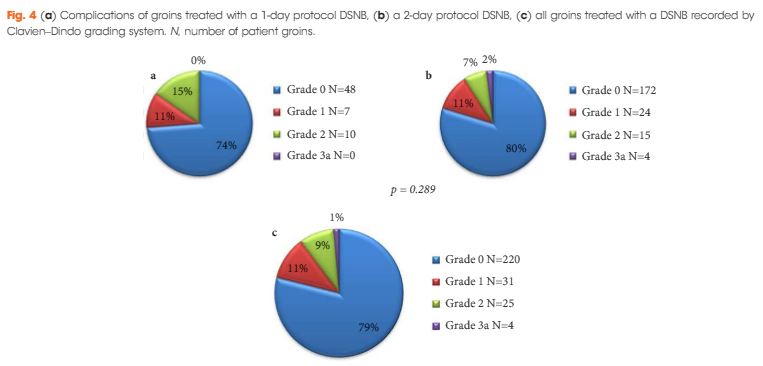
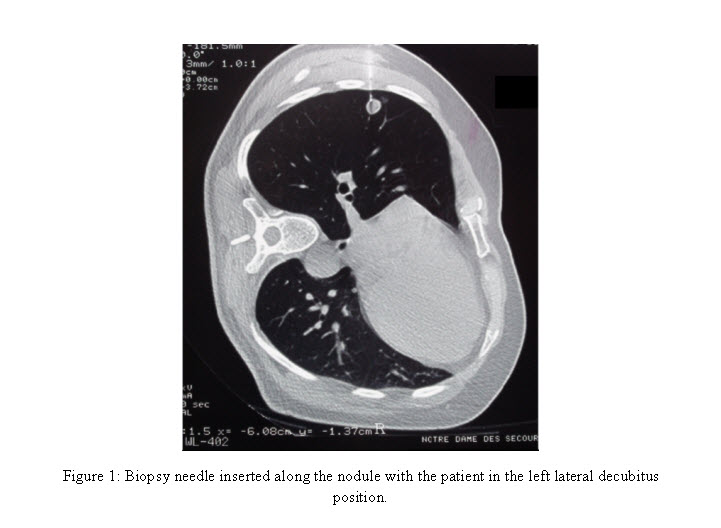
After signing the informed consent, the biopsy was performed under local anaesthesia, with the patient inthe left lateral decubitusposition. A 15 cm; 18 G automated cutting needle was inserted into the lesion with a single step approach during a single breath hold. Within the procedure the patient was totally co-operative; he didn’t cough or breath inappropriately (fig 1). The needle was removed during a second breath hold.
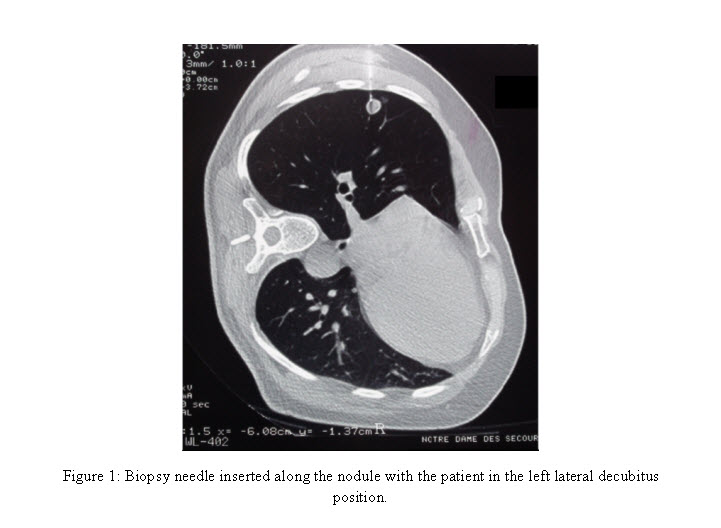
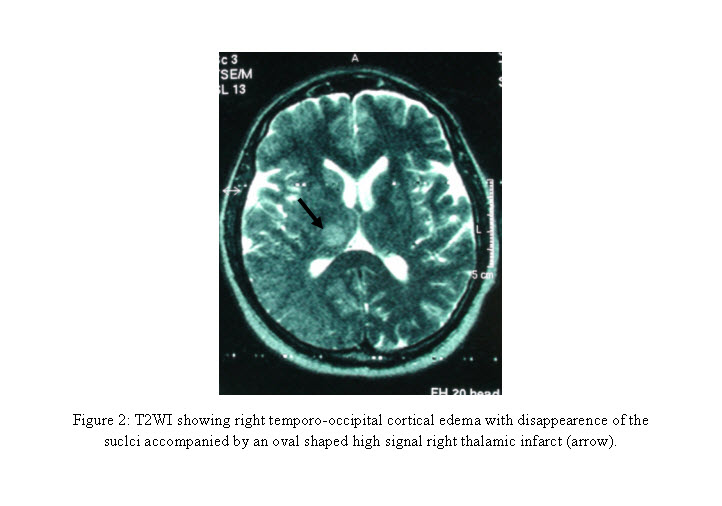
Just after the completion of the nodule biopsy, the patient developed a generalized tonico-clonic seizure then became unresponsive. Immediate resuscitation was started;a100% oxygen mask ventilation was placed and the cardiac arrest team was called. The patient regained consciousness, with persistent somnolence and left hemiplegia. An urgent brain CT scan performed without IV contrast administration revealed no abnormalities, but as the clinical course suggested a serious injury, a brain MRI was performed 1 hour later. This revealed a tiny cortical infarction in the area of the right posterior cerebral artery demonstrated on the Diffusion Weighted Images (fig 2). The patient had a full recovery after 100% oxygentherapy. No hyperbaric oxygen treatment was needed.
The histopathologic exam confirmed the metastatic nature of the lung nodule consistent with the primary NSGCT.
Discussion
Percutaneous transthoracic needle biopsy is nowadays a ‘must’ procedure for evaluating lung lesions. Air embolism is a rare unpredictable complication but potentially fatal. The incidence of a systemic air embolism is probably underestimateddue to asymptomatic patients. Different studies suggested that air embolism induces endothelial damage, activating a thrombo-inflammatory process responsible of micro thrombus creation2.
Once in the vascular circulation, the gas follows the blood flow until it get blocked in the small vessels. Even a small air volume can occlude distal arteries. The clinical symptoms depend primarily on the territory of the microvascular obstruction. In fact, the presence of air within the spinal cord arteries is responsible foran electrical discharge sensation in the legs facilitated by the prone position, as these arteries arise from the intercostal or lumbar arteries themselves arising from the posterior and postero-lateral wall of the aorta3.If an air embolism reached the coronary arteries, arrhythmia, ischaemia and myocardial infarction could occur.Whereas, if it reached the cerebral arteries,focal neurologic deficit, hemiplegia, seizures, coma and even death were probable.
There are mainly three possible ways for air to be introduced into the pulmonary venous system during PTNB4. Air may enter directly through the needle tip placed into a pulmonary vein with an open ended base to the atmospheric pressure, which exceeds the pulmonary venous pressure during deep inspiration. In our case, this is not possible since no coaxial needle was used. Also, a needle may simultaneously penetrate an air containing space nearby a pulmonary vein, since coughing orvalsalvamanoeuvre may increase the airway pressure, facilitating the aspiration of air into the pulmonary vein5, 6. Again our patient was very compliant to our requests- he didn’t cough during the procedure but a valsalva cannot be ruled out. Finally, a communication between the bronchus and a pulmonary vein may be responsible of air passage.If a transient fistula is created when the needle is passing through the lung parenchyma, intraalveolar or intrabronchial air might be introduced into the pulmonary vein. This mechanism could have taken place in our case.
The clinical diagnosis is based on the sudden neurologic and/or cardiovascular symptoms occurring just after the biopsy. Computed tomography may confirm the diagnosis, showing air bubbles in the coronary arteries, the cerebral circulation, the cardiac cavities or the aorta. Once the diagnosis is suspected, immediate treatment by a 100% Oxygen mask and transfer to a hyperbaric air Oxygen chamber is crucial,in order to reduce the gas bubble size replacing nitrogen with Oxygen, and restoring circulation and tissue oxygenation7.
Unfortunately, our institution does not possess a hyperbaric oxygen treatment and the patient was not transferred to another institution for this treatment, given the rapid favorable progress-probably due to the very small gas volume embolism, and rapid commencement of 100% oxygenation.
Although air embolism is a rare complication associated with PTNB, it has been reported previously. Interventional radiology services should consider having in place a clinical protocol applicable toPTNB, to handle this very rare but life threatening complication of arterial air embolism, thereby optimisingoutcome , since the histopathologic nature of such nodule in such categories of patients is the key point for the subsequent management.
References
1- Sinner WN. Complications of percutaneous transthoracic needle aspiration biopsy. ActaRadiolDiag 1976; 17: 813-28
2- HsiDH, ThompsonTN, FreatherA, et al. Simultaneous coronary and cerebral air embolism after CT-guided core needle biopsy of the lung. Tex Heart Enst J. 2008; 35(4): 472-474.
3- Muth CM, Shank ES. Gas Embolism. N Engl J Med 2000; 342:476-482
4- Hiraki T, Fujiwara H, Sakurai J, et al. Non fatal systemic air embolism complicating percutaneous CT-guided transthoracic needle biopsy: four cases from a single institution. Chest 2007; 132: 684 – 690
5- Wescott JL. Air embolism complicating percutaneous needle biopsy of the lung. Chest 1973; 63: 108 – 110
6- Baker BK, Awwad EE. Computed tomography of fatal cerebral air embolism following percutaneous aspiration biopsy of the lung. J comput Assist Tomogr 1988; 12: 1082 – 1083
7- Lattin G, O’Brien W Sr, Mc Cray B, et al. Massive systemic air embolism treated with hyperbaric oxygen therapy following CT-guided transthoracic needle biopsy of a pulmonary nodule. J VascIntervRadiol 2006; 17: 1355-1358
Date added to bjui.org: 09/11/2012
DOI: 10.1002/BJUIw-2012-053-web