Residents’ podcast: NICE guidelines – renal and ureteric stones
Nikita Bhatt is a Specialist Trainee in Urology in the East of England Deanery and a BURST Committee member @BURSTUrology
NICE Guideline – Renal and ureteric stones: assessment and management
Context
Renal and ureteric stones usually present as an acute episode with severe pain, although some stones are picked up incidentally during imaging or may present as a history of infection. The initial diagnosis is made by taking a clinical history and examination and carrying out imaging; initial management is with painkillers and treatment of any infection.
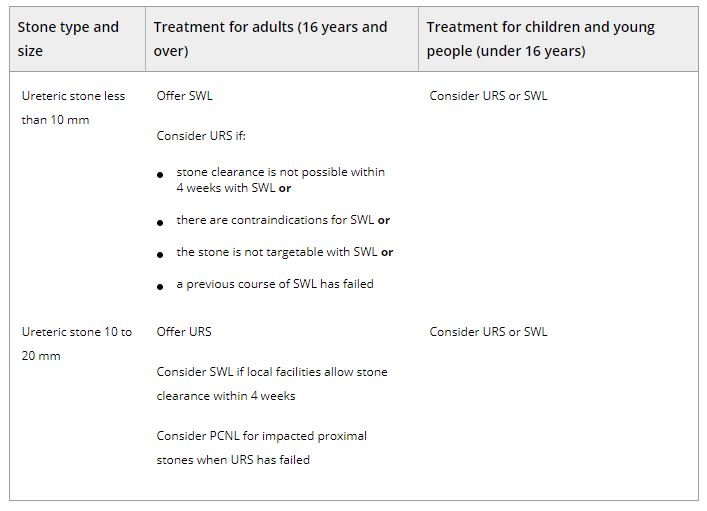
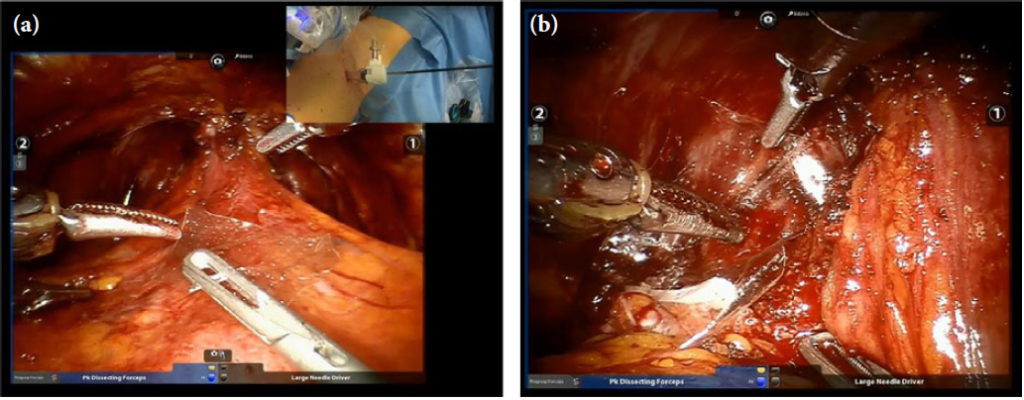
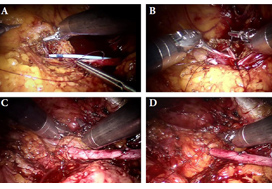
Ongoing treatment of renal and ureteric stones depends on the site of the stone and size of the stone (less than 10 mm, 10 to 20 mm, greater than 20 mm; staghorn stones). Options for treatment range from observation with pain relief to surgical intervention. Open surgery is performed very infrequently; most surgical stone management is minimally invasive and the interventions include shockwave lithotripsy (SWL), ureteroscopy (URS) and percutaneous stone removal (surgery). As well as the site and size of the stone, treatment also depends on local facilities and expertise. Most centres have access to SWL, but many use a mobile machine on a sessional basis rather than a fixed‐site machine, which has easier access during the working week. The use of a mobile machine may affect options for emergency treatment, but may also add to waiting times for non‐emergency treatment.
Although URS for renal and ureteric stones is increasing (there has been a 49% increase from 12,062 treatments in 2009/10, to 18,066 in 2014/15 [Hospital Episode Statistics data]), there is a trend towards day‐case/ambulatory care, with this increasing by 10% to 31,000 cases a year between 2010 and 2015. The total number of bed‐days used for renal stone disease has fallen by 15% since 2009/10. However, waiting times for treatment are increasing and this means that patient satisfaction is likely to be lower.
Because the incidence of renal and ureteric stones and the rate of intervention are increasing, there is a need to reduce recurrences through patient education and lifestyle changes. Assessing dietary factors and changing lifestyle have been shown to reduce the number of episodes in people with renal stone disease.
Adults, children and young people using services, their families and carers, and the public will be able to use the guideline to find out more about what NICE recommends, and help them make decisions. These recommendations apply to all settings in which NHS‐commissioned care is provided.
Table 2.Surgical treatment (including SWL) of ureteric stones in adults, children and young people Abbreviations: PCNL, percutaneous nephrolithotomy; SWL, shockwave lithotripsy; URS, ureteroscopy.
BJUI Podcasts now available on iTunes, subscribe here https://itunes.apple.com/gb/podcast/bju-international/id1309570262