Editorial: Can artificial intelligence optimize case selection for hemi‐gland ablation?
The victory of ‘AlphaGo’ over humans in Go, one of the most complex games with more than 10170 board configurations, has yielded tremendous attention worldwide [1]. The later version, ‘AlphaGo Zero’, has brought artificial intelligence (AI) to the next level by demonstrating an absolute superiority, winning 100‐0 against the champion‐defeating AlphaGo [2]. It is exciting, and perhaps shocking, to realize what AI can achieve.
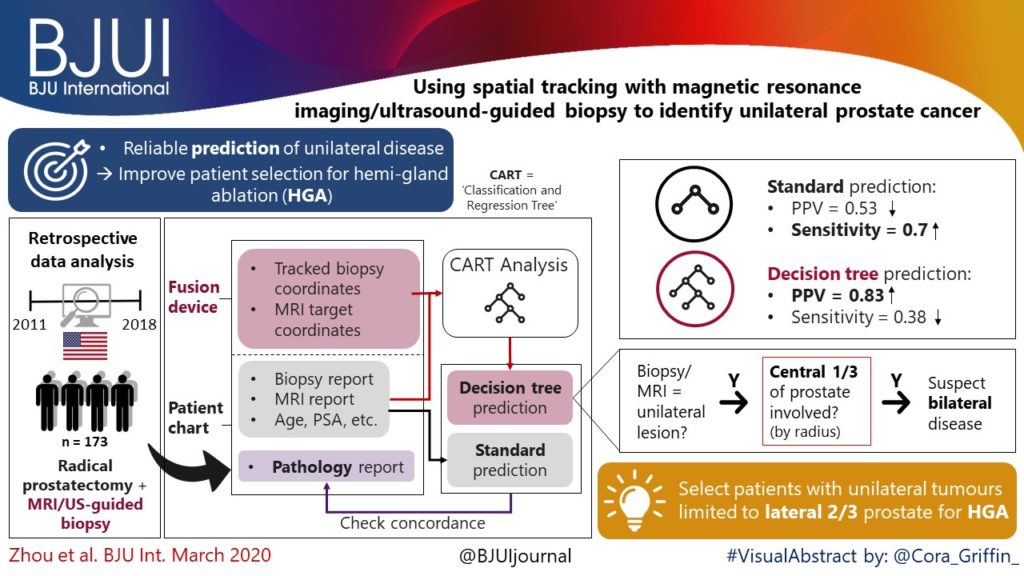
In this issue of BJUI, the study by Zhou et al. [3] is the first to utilize AI to optimize case selection for hemi‐gland ablation. In this study, classification and regression tree (CART) analysis, which is a form of supervised machine‐learning algorithm, was used to identify laterality of prostate cancer. In the conventional approach, case selection was based on biopsy results and MRI findings. For the CART model, in addition to the common clinical variables (i.e. age, PSA, prostate volume, biopsy and MRI results), biopsy coordinate‐derived spatial features were also used as model inputs. The model output was the probability of unilateral clinically significant prostate cancer considered suitable for hemi‐gland ablation. Whole‐mount prostatectomy specimens were used as the standard of reference. The CART model correctly identified laterality in 80% of the cases, compared to 73% with the conventional approach. The positive predictive value of the CART model was 83%, compared to 53% with the conventional approach. The superiority of the CART model has been demonstrated, and the area under curve was 0.82.
Artifical intelligence has been widely adopted in the field of Urology [4]. For prostate cancer detection in particular, our group evaluated the diagnostic performances of four machine‐learning models based on clinical variables in a biopsy cohort of 1625 men [5]. The machine‐learning models achieved excellent performances in detecting clinically significant prostate cancer, with an accuracy of up to 95.3%. Algohary et al. [6] constructed three machine‐learning models to identify the presence of clinically significant prostate cancer based on MRI radiomic features in patients who underwent active surveillance. When compared with the Prostate Imaging–Reporting and Data System (PI‐RADS) scoring system, the machine‐learning models were able to improve overall accuracy by 30–80%.
Fehr et al. [7] developed an automated system to classify Gleason scores based on MRI images. The automated system could distinguish between Gleason scores of 6 and 7 or above cancers with an accuracy of up to 93%. The differentiation between Gleason score 3+4 and 4+3 disease also yielded an accuracy of up to 93%. Importantly, the performance of AI and machine‐learning models is highly dependent on the quality and accuracy of the data being input. In terms of prostate cancer detection, either mapping biopsy or whole‐mount prostatectomy specimens should be considered to represent the ‘ground truth’.
There are a number of challenges in implementing AI in clinical practice. First, decision‐making in healthcare requires logical deduction and explanation. The data processing in AI, however, is often described as a ‘black box’. Taking AlphaGo as an example, some ‘moves’ were considered incomprehensible even by world‐class players. Second, although results from AI are promising, there is in general a lack of regulations and standards to assess its safety, efficacy and validity. Liability issues can be problematic in case of medical mishaps. Third, doctors are human. Conflict of interest does exist, and how we can utilize AI in a complementary rather than a competitive manner is a challenging obstacle to overcome.
Nevertheless, AI has huge potential in improving healthcare. Collaborative effort is needed globally to develop and optimize AI systems, and to increase its acceptability and practicality upon implementation. Future studies answering clinically important questions using appropriate standards of reference will be of paramount importance in paving the way for the AI era in urology.
by Jeremy Yuen‐Chun Teoh, Edmund Chiong and Chi‐Fai Ng
References
- , , et al. Mastering the game of Go with deep neural networks and tree search. Nature 2016; 529: 484– 9
- , , et al. Mastering the game of Go without human knowledge. Nature 2017; 550: 354– 9
- , , et al. Using spatial tracking with magnetic resonance imaging/ultrasound‐guided biopsy to identify unilateral prostate cancer. BJU Int 2020; 125: 399– 406
- , , et al. Current status of artificial intelligence applications in urology and their potential to influence clinical practice. BJU Int 2019; 124: 567– 77
- , , . Diagnosis of prostate cancer in a Chinese population by using machine learning methods. Conf Proc IEEE Eng Med Biol Soc 2018; 2018: 1– 4
- , , et al. Radiomic features on MRI enable risk categorization of prostate cancer patients on active surveillance: Preliminary findings. J Magn Reson Imaging 2018; 48: 818– 28
- , , et al. Automatic classification of prostate cancer Gleason scores from multiparametric magnetic resonance images. Proc Natl Acad Sci USA 2015; 112: E6265– 73