Video: BJUI Compass: what’s your favourite paper?
Former BJUI Compass Editor, Dr John Davis, in discussion with Dr Janet Kukreja about her recent favourite papers assessed for the journal.
Former BJUI Compass Editor, Dr John Davis, in discussion with Dr Janet Kukreja about her recent favourite papers assessed for the journal.
Paediatric urologist Antonio Macedo, author of e-learning module Postnatal bladder function after in utero repair of myelomeningocele: a literature review talks to Stephen Griffin.
BJUI Knowledge: The CPD portal for urologists
Comprehensive, trustworthy and easy to use e-learning platform for trainees, residents, consultants and all specialising in urology.
BJUI Knowledge is evidence-based, fully referenced and peer reviewed to ensure academic, scientific and editorial validity.
Author Monique Roobol talks to associate editor Greg Shaw about screening for prostate cancer.
BJUI Knowledge: The CPD portal for urologists
Comprehensive, trustworthy and easy to use e-learning platform for trainees, residents, consultants and all specialising in urology.
BJUI Knowledge is evidence-based, fully referenced and peer reviewed to ensure academic, scientific and editorial validity.
We would particularly like to thank the following individuals who are the top reviewers for the journal in 2020, all with ≥10 reviews
| Nathan Lawrentschuk | Sima Porten |
| Tobias Klatte | Roderick van den Bergh |
| Sigrid Carlsson | Stephan Madersbacher |
| Riccardo Autorino | Niranjan Sathianathen |
| Matthew Roberts | Yair Lotan |
| Alexander Cole | Asif Muneer |
We are extremely grateful to all our reviewers for their time and hard work during an incredibly difficult year
| Aastha | Abdollah, Firas | Abel, E. | Abouassaly, Robert |
| Abrams, Paul | Abreu, Leonardo | Acher, Peter | Adolfsson, Jan |
| Adshead, James | Ahdoot, Michael | Ahlawat, Rajesh | Ahlgren, Johan |
| Ahluwalia, Puneet | Ahmad, Imran | Ahmed, Hashim | Ahmed, Kamran |
| Aho, Tev | Ajayi, Leye | Al Jaafari, Feras | Alam, Ridwan |
| Albersen, Maarten | Albertsen, Peter | Alhasso, Ammar | Alifrangis, Constantine |
| Allaway, Matthew | Aloj, Luigi | Alzweri, Laith | Aminsharifi, Alireza |
| Anderson, Christopher | Anderson, Mark | Anderson, Paul | Andolfi, Ciro |
| Antonelli, Jodi | Apostolidis, Apostolos | Armitage, James | Arndt, Volker |
| Arora, Sohrab | Arsov, Christian | Ashrafi, Akbar | Assimos, Dean |
| Averbeck, Marcio | Aydin, Abdullatif | Baack Kukreja, Janet | Baard, Joyce |
| Babjuk, Marek | Badlani, Gopal H. | Bahnson, Robert | Bajic, Petar |
| Bajpai, Minu | Balasubramanian, Adithya | Ball, Mark | Bandini, Marco |
| Bangma, Chris | Barber, Neil | Barod, Ravi | Barrett, Tristan |
| Baumgarten, Adam | Beard, David | Becerra, Maria | Becher, Edgardo |
| Bedke, Jens | Behre, Hermann | Beisland, Christian | Belenchon, Ines |
| Bell, Richard | Berglund, Anders | Betschart, Cornelia | Bex, Axel |
| Bhandari, Mahendra | Bhat, Seetharam | Bhatt, Jaimin | Bhatt, Nikita |
| Bhindi, Bimal | Bianchi, Daniele | Bianchi, Lorenzo | Birkhäuser, Frédéric |
| Birkhäuser, Veronika | Biyani, Chandra | Bjartell, Anders | Blackmur, James |
| Blazeby, Jane | Blecher, Gideon | Blick, Christopher | Blok, Bertil |
| Bloom, Jonathan | Boddy, Jane | Bogaert, Guy | Bokhorst, Leonard |
| Bolgeri, Marco | Bolton, Damien | Boone, Timothy | Borkowska, Edyta |
| Bose, Pradeep | Boström, Peter | Bratt, Ola | Brehmer, Marianne |
| Brewin, James | Brewster, Simon | Briganti, Alberto | Bromage, Steve |
| Brooks, Nathan | Brouwer, Oscar | Brown, Christian | Brown, Matthew |
| Bryan, Richard | Bryant, Richard | Budäus, Lars | Buffi, Nicolò |
| Bukavina, Laura | Bultitude, Matthew | Burgu, Berk | Burkhard, Fiona |
| Butler, Santino | Butow, Phyllis | Byrne, Fiona | Cadeddu, Jeffrey |
| Cahill, Declan | Cai, Tommaso | Caldamone, Anthony | Camilleri, Philip |
| Campbell, Jeffrey | Campeau, Lysanne | Campi, Riccardo | Canda, Abdullah Erdem |
| Canning, Douglas | Cantiello, Francesco | Capitanio, Umberto | Capogrosso, Paolo |
| Cardozo, Linda | Carlo, Buonerba | Caroppo, Ettore | Castiglione, Fabio |
| Castro-Diaz, David | Cathcart, Paul | Celia, Antonio | Cellek, Selim |
| Cerruto, Maria Angela | Challacombe, Ben | Chancellor, Michael | Chander, Sarat |
| Chandra, Ashish | Chandra, Lizzie | Chandrasekar, Thenappan | Chang, David |
| Chapin, Brian | Chapple, Christopher | Chatta, Gurkamal | Checcucci, Enrico |
| Chee, Justin | Cheung, Douglas | Chew, Ben | Chi, Thomas |
| Chin, Joseph | Chin, Kwang | Chin, Peter | Chin, Stephen |
| Chow, Ken | Christopher, Nim | Chuang, Yao-Chi | Chun, Felix |
| Chung, Doreen | Chung, Eric | Clark, Jack | Clemens, J. Quentin |
| Cohen, Ronald | Collins, Justin | Colquhoun, Alexandra | Compérat, Eva |
| Cone, Eugene | Coode-Bate, Jack | Cooper, Colin | Corcoran, Niall |
| Corcos, Jacques | Cosker, Thomas | Costello, Anthony | Cotterill, Nikki |
| Cox, Edward | Crabb, Simon | Cracco, Cecilia | Cranston, David |
| Cresswell, Joanne | Crockett, Matthew | Cross, Brian | Cruz, Célia |
| Cruz, Francisco | Cui, Helen | Culig, Zoran | Cullen, Victoria |
| Cumberbatch, Marcus | Cutress, Mark | Cuypers, Maarten | Cynk, Mark |
| Da Ros, Carlos | Dabestani, Saeed | Dahm, Philipp | Dan, Woodcock |
| D’Andrea, David | Daneshmand, Siamak | Danila, Daniel | Danuser, Hansjoerg |
| Darr, Christopher | Dasgupta, Ranan | Dauw, Casey | Davies, Lucy |
| Davis, John | De Giorgi, Ugo | de la Taille, Alexandre | De Meerleer, Gert |
| De Reijke, Theo M. | De Win, Gunter | Del Popolo, Giulio | D’Elia, Carolina |
| Dell’Oglio, Paolo | Delprado, Warick | Denstedt, John | Derweesh, Ithaar |
| Desai, Janak | Desai, Mahesh | Diamond, David | Dinkelman-Smit, M. |
| Dmochowski, Roger | Doizi, Steeve | Donovan, Jenny | Dragos, Laurian |
| Drake, Marcus | Droupy, Stéphane | Dudderidge, Tim | Dukic, Ivo |
| Dundee, Philip | Eapen, Renu | Eardley, Ian | Eastham, James |
| Eberli, Daniel | Eddy, Ben | Eden, Christopher | Egawa, Shin |
| Egevad, Lars | Ehdaie, Behfar | Eichler, Martin | Eisenberger, Mario |
| Eisner, Brian | Elders, Andrew | Eldred-Evans, David | Elhage, Oussama |
| Ellis, Robert | Elmamoun, Mamoun | Elneil, Sohier | Elsamra, Sammy |
| Elshal, Ahmed | Elterman, Dean | Emberton, Mark | Engeler, Daniel |
| Enikeev, Dmitry | Enting, Deborah | Epstein, Jonathan | Erickson, Andrew |
| Escudero, Lorena | Eure, Gregg | Everaert, Karel | Everaerts, Wouter |
| Eversden, Elizabeth | Eyre, David | Falagario, Ugo | Falcone, Marco |
| Faltas, Bishoy | Feber, Andrew | Fero, Katherine | Ferro, Matteo |
| Ficarra, Vincenzo | Fife, Kate | Finazzi Agrò, Enrico | Finch, William |
| Fletcher, Sean | Fojecki, Grzegorz | Friedlander, David | Frydenberg, Mark |
| Furr, James | Furrer, Marc | G. Zaorsky, Nicholas | Gacci, Mauro |
| Gadzhiev, Nariman | Gadzinski, Adam | Gakis, Georgios | Galfano, Antonio |
| Gall, Zara | Gallagher, Kevin | Gallieni, Maurizio | Gandaglia, Giorgio |
| Gao, Chuanyu | Gearhart, John | Geavlete, Petrisor | Georgiades, Fanourios |
| Geurts, Nicolas | Ghai, Sangeet | Ghani, Khurshid | Ghazi, Ahmed |
| Gianduzzo, Troy | Giannantoni, Antonella | Gietzmann, William | Giganti, Francesco |
| Gilbert, James | Gild, Philipp | Giusti, Guido | Gnanapragasam, Vincent |
| Goldenberg, Larry | Goldman, Howard | Goldsmith, Louise | Golla, Vishnukamal |
| Gomes, Cristiano | Gontero, Paulo | Good, Daniel | Goonewardene, Sanchia |
| Gordon, Stephen | Gorin, Michael | Graefen, Markus | Granr, Aurelie |
| Gravas, Stavros | Gregg, Justin | Grilo, Nuno | Groen, Jan |
| Gross, Oliver | Gross, Tobias | Grummet, Jeremy | Gulati, Roman |
| Gurney, Howard | Guru, Khurshid | Guruli, Georgi | Ha, Yun-Sok |
| Hackett, Geoff | Hakenberg, Oliver | Hakimi, A Ari | Hamid, Rizwan |
| Hamm, Rebecca | Han, Deok Hyun | Han, Ping | Handelsman, David |
| Hasan, Mudhar | Hashad, Mohamed Mohie Eldin | Hashimoto, Takeshi | Hatakeyama, Shingo |
| Haug, Alexander | Häuser, Lorine | Hautmann, Richard E. | Hayne, Dickon |
| Heck, Matthias | Heer, Rakesh | Hegarty, Paul K. | Heidenreich, Axel |
| Heijnsdijk, Eveline | Helfand, Brian | Heller, Nick | Hellstrom, Wayne |
| Henderson, John | Hendry, Rob | Henry, Ann | Hensley, Patrick |
| Herkommer, Kathleen | Hermanns, Thomas | Herrmann, Thomas | Hindley, Richard |
| Hofman, Michael | Hollingsworth, John | Holmberg, Lars | Hosseini, Abolfazl |
| Houédé, Nadine | Hounsome, Luke | Hovens, Chris | Howles, Sarah |
| Hu, Jim | Hughes, Simon | Hulson, Oliver | Humphreys, Mitchell |
| Hung, Andrew | Husmann, Douglas | Hutel, Michael | Hwang, Eu Chang |
| Igawa, Yasuhiko | Ilg, Marcus | Innos, Kaire | Ishioka, Junichiro |
| Jambor, Ivan | JC, Liao | Johnson, Mark | Johnston, Thomas |
| Jonasch, Eric | Jones, James | Joseph, Jean | Joyce, Adrian |
| Jung, Helene | Jung, Jae Hung | Junker, Kerstin | Kalejaiye, Ayo |
| Kamal, Wissam | Kamat, Ashish | Kamphuis, Guido | Kaouk, Jihad |
| Kaplan, Steven | Karakiewicz, Pierre | Karam, Jose | Karnes, R |
| Kasivisvanathan, Veeru | Kassouf, Wassim | Kastner, Christof | Kates, Max |
| Kattan, Mike | KAYA, ENGIN | Kayes, Oliver | Keam, Simon |
| Keanie, Julian | Keeley, Frank | Kekre, Nitin | Keoghane, Stephen |
| Kessler, Thomas | Khaki, Ali | Khan, Muhammad Shamim | Khetrapal, Pramit |
| Khochikar, Makarand | Kim, Hyung | Kim, Isaac | Kimura, Shoji |
| Kirsch, Andrew J. | Kishida, Takeshi | Kiss, Bernhard | Kitta, Takeya |
| Klein, Eric | Klein, Robert | Kliesch, Sabine | Klotz, Laurence |
| Kneebone, Andrew | Knight, Simon | Knipper, Sophie | Knoll, Thomas |
| Knudsen, Bodo | Kobayashi, Takashi | Kockelbergh, Roger | KOGA, Fumitaka |
| Kondo, Tsunenori | Konety, Badrinath | Koo, Kyo Chul | Korte, James |
| Kosmoliaptsis, Vasilis | Kotb, Ahmed | Kovac, Evan | Kozomara, Marko |
| Krambeck, Amy | Kramer, Mario | Kretschmer, Alexander | Kriegmair, Maximilian |
| Kroeger, Nils | Krokidis, Miltos | Kulkarni, Meghana | Kulkarni, Sanjay |
| Kumar, Sunil | Kumar, Vivekanandan | Kundu, Bibhas | Kuo, Hann-Chorng |
| Kurithof-de Julio, Marianna | Kutikov, Alex | Kwan, Edmond | Laguna, Pilar |
| Laird, Alexander | Lallas, Costas | Lam, Thomas | Lam, Wayne |
| Lamb, Alastair | Lamb, Benjamin | Landman, Jaime | Langenhuijsen, Johan |
| Lantz, Anna | Larcher, Alessandro | Lascano, Danny | Laurentino, Sandra |
| Le Roux, Pieter | Lec, Patrick | Lee, Eugene | Lee, Wai Gin |
| Leiber, Christian | Leitner, Lorenz | Lenfant, Louis | Lenis, Andrew |
| Leow, Jeffrey | Leppert, John | Lerner, Lori | Leung, Steve |
| Levine, Larry | Lewington, Andrew | Leyh-Bannurah, Sami-Ramzi | Liatsikos, Evangelos |
| Liau, Siong | Lilja, Hans | Liow, Elizabeth | Lipkin, Michael |
| Lipshultz, Larry | Liu, Jui-Ming | Lo, Simon | Loblaw, Andrew |
| Loeb, Stacy | Lonergan, Peter | Lopez, Francisco | Lopez-Beltran, Antonio |
| Louie, Alexander | Louie-Johnsun, Mark | Love, Christopher | Lovegrove, Catherine |
| Lucca, Ilaria | Lughezzani, Giovanni | Luiting, Henk | Luk, Angus |
| Luo, Jun | Luzzago, Stefano | Ma, Runzhuo | MacLennan, Sara |
| MacPherson, Ruth | Madaan, Sanjeev | Madersbacher, Helmut | Magee, Diana |
| Mahal, Brandon | Malde, Sachin | Manecksha, Rustom | Manley, Brandon |
| Mantica, Guglielmo | Marchioni, Michele | Margulis, Vitaly | Mari, Andrea |
| Mariappan, Paramananthan | Mariotti, Guilherme | Mark, Stephen | Marks, Leonard |
| Marra, Giancarlo | Marshall, Ernie | Martin, Richard | Martini, Alberto |
| Masson-Lecomte, Alexandra | Masterson, Timothy | Matanhelia, Mudit | Matin, Surena |
| Matsumoto, Kazuhiro | Mattei, Agostino | Maurer, Tobias | Mazhar, Danish |
| Mazzone, Elio | McCaig, Fiona | McGrath, John | Mcintosh, lachlan |
| McNeill, Alan | Mehan, Nicholas | Mehnert, Ulrich | Mehrazin, Reza |
| Meijer, Richard | Mejean, Arnaud | Mendichovszky, Iosif | Meng, Maxwell |
| Menogue, Stuart | Menon, Mani | Merseburger, Axel | Mertens, Laura |
| Meyer, Christian | Miah, Saiful | Michel, Martin | Michels, Lars |
| Miernik, Arkadiusz | Millar, Jeremy | Miller, Eric | Miller, Nipor |
| Mills, Ian | Minhas, Suks | Mir, Maria | Mistretta, Francesco |
| Mitchell, Catherine | Mitchell, Tom | Mitin, Timur | Mitra, Anirban |
| Moch, Holger | Molden-Hauer, Tristan | Molina-Garrido, Maria-Jose | Monastyrskaya, Katia |
| Monn, M Francesca | Montorsi, Francesco | Moon, Daniel | Moore, Caroline |
| Moore, Katherine | Mordasini, Livio | Moretti, Kim | Morita, Masashi |
| Moschini, Marco | Moschovas, Marcio | Mossanen, Matthew | Mostafid, Hugh |
| Muhitch, Jason | Mühlstädt, Sandra | Muir, Gordon | Mukhopadhyay, Subhankar |
| Mulders, Peter | Mumtaz, Faiz | Mundy, Anthony | Murphy, Declan |
| Murray, Julia | Murray, Katie | Murtola, Teemu | Musco, Stefania |
| Mushtaq, Imran | Mynbaev, Ospan | Nabi, Ghulam | Nabi, Junaid |
| Nair, Rajesh | Namdarian, Benjamin | Narayan, Vikram | Nathan, Senthil |
| Neal, Naomi | Necchi, Andrea | Nelson, Adam | Netsch, Christopher |
| Neumeier, Vera | Neves, Joana | Nguyen, David-Dan | Nguyen, Hao |
| Nichol, David | Nickel, J. Curtis | Nicol, David | Nieboer, Daan |
| Nieto, Yago | Nobrega, Richard | Nonomura, Norio | Nordhoff, Verena |
| Nottingham, Charles | Nyame, Yaw | Nzenza, Tatenda | Oades, Grenville |
| O’Brien, Tim | O’Brien, Timothy | O’Connor, Kevin | Oddens, Jorg |
| Oh, William | Olsburgh, Jonathon | Omer, Altan | Ong, Wee |
| Osses, Daniël | Osther, Palle | O’Sullivan, Richard | Oudard, Stéphane |
| Ouzaid, Idir | Paciotti, Marco | Page, Toby | Pal, Sumanta |
| Paller, Channing | Panebianco, Valeria | Panicker, Jalesh | Pannek, Jürgen |
| Pantuck, Allan | Pariser, Joseph | Parker, Chris | Parnham, Arie |
| Partin, Alan | Pasquier, David | Patel, Hiten | Patel, Keval |
| Patel, Manish | Patel, Parth | Patel, Uday | Patel, Vipul |
| Patil, Vishal | Patki, Prasad | Patterson, Jake | Pavlovich, Christian |
| Payne, Steve | Pearce, Ian | Pearle, Margaret | Pecoraro, Angela |
| Penzkofer, Tobias | Perera, Marlon | Perez Fentes, Daniel | Pérez, Daniel |
| Peters, Craig | Peters, Inga | Peters, Max | Petros, Firas |
| Pettaway, Curtis | Peyronnet, Benoit | Pfail, John | Pfister, David |
| Phé, Véronique | Philip, Stuart | Pierorazio, Phillip | Ploumidis, Achilles |
| Pokorny, Morgan | Pontari, Mike | Pook, David | Popert, Richard |
| Porcaro, Antonio | Porpiglia, Francesco | Porter, James | Portis, Andrew |
| Poulsen, Mads | Pradere, Benjamin | Preminger, Glenn | Presicce, Fabrizio |
| Preston, Mark | Proietti, Silvia | Protheroe, Andrew | Pryor, David |
| Quarrier, Scott | Radtke, Jan Philipp | Ragab, Mostafa | Rai, Bhavan |
| Raison, Nicholas | Rajan, Prabhakar | Rajan, Probhakaran | Rakauskas, Arnas |
| Ralph, David | Ramakrishnan, Venkat | Ramasamy, Ranjith | Ranasinghe, Weranja |
| Rane, Abhay | Rannikko, Antti | Rashid, Aso Omer | Rashid, Prem |
| Rassweiler, Jens | Rastinehad, Ardeshir | Ratan, Hari | Ratliff, Timothy |
| Rawal, Sudhir | Razvi, Hassan | Rees, Rowland | Reeves, Fairleigh |
| Rehder, Peter | Reisman, Yacov | Reiter, Robert | Remzi, Mesut |
| Reynard, John | Richenberg, Jonathan | Rider, Jennifer | Rieken, Malte |
| Riggs, Stephen | Rimmer, Yvonne | Rink, Michael | Roberts, William |
| Robinson, Brian | Robinson, Dudley | Robson, Craig | Rocco, Bernardo |
| Rochester, Mark | Roehrborn, Claus | Rogers, Craig | Roghmann, Florian |
| Rolevich, Alexander | Romero Otero, Javier | Rosario, Derek | Rosier, Peter |
| Ross, Ashley | Rossi, Sabrina | Rottenberg, Giles | Rovito, Michael |
| Rowe, Courtney | Ruiz-Castañe, Eduardo | Rukin, Nicholas | Russell, Neil |
| Russo, Giorgio Ivan | Russo, Paul | Sabnis, Ravindra | Sadeghi, Ramin |
| Sadeghi-Nejad, Hossein | Saeb-Parsy, Kasra | Sahai, Arun | Salami, Simpa |
| Salmon, Jonathan | Salonia, Andrea | Sammon, Jesse | Sanchez-Salas, Rafael |
| Sangster, Philippa | Sansone, Andrea | Sarma, Aruna | Satasivam, Prassannah |
| Satkunasivam, Raj | Savovic, Jelena | Schagdarsurengin, Undraga | Schalken, Jack |
| Schartau, Patricia | Scheiner, David | Schenk, Jeannette | Schmitz-Dräger, Bernd |
| Schneider, Florian | Schneider, Marc | Schurch, Brigitte | Scriven, Sharon |
| Seisen, Thomas | Sengupta, Shomik | Sethi, Kapil | Sethia, Krishna |
| Sfakianos, John | Shabbir, Majed | Shabbir, Majid | Shah, Amishi |
| Shapiro, Daniel | Sharma, Gyanendra | Shaw, Greg | Sheinfeld, Joel |
| Shi, Zhongjie | Shiradkar, Rakesh | Shoag, Jonathan | Shoji, Sunao |
| Siddiqui, M | Sievert, Karl-Dietrich | Singla, Nirmish | Siva, Shankar |
| Skipworth, Richard | Skolarus, Ted | Smith, Angela | Smith, Phillip |
| Smyth, Lisa | Soares, Ricardo | Soave, Armin | Soloway, Mark |
| Somani, Bhaskar | Sonn, Geoffrey | Sood, Akshay | Soomro, Naeem |
| Sooriakumaran, Prasanna | Soria, Francesco | Sotelo, Rene | Speakman, Mark |
| Speakman, MJ | Spiess, Phillippe | Sprenkle, Preston | Srinivasan, Arun |
| Sripathi, Venkat | Sriprasad, Seshadri | Staehler, Michael | Stai, Bethany |
| Stamatiou, Konstantinos | Stark, Dan | Stattin, Pär | Stenzl, Arnulf |
| Steuber, Thomas | Steyerberg, Ewout | Stillebroer, Alexander | Stinesen Kollberg, Karin |
| Stish, Bradley | Stockler, Martin | Stoffel, John | Stolzenburg, Jens-Uwe |
| Stone, Nelson | Stratton, Kelly | Strebel, Räto | Stricker, Phillip |
| Sturch, Paul | Suarez, Rodrigo | Subramaniam, Ramnath | Sullivan, Mark |
| Sur, Roger | Taghizadeh, Arash | Takeda, Toshikazu | Tan, Hung-Jui |
| Tan, Wei Shen | Tandogdu, Zafer | Tang, Chad | Teh, Jiasian |
| Tekgul, Serdar | Teoh, Jeremy | Terris, Martha K. | Tewari, Ash |
| Thalmann, George | Thiruchelvam, Nikesh | Thomas, Charalampos | Thomas, Johanna |
| Thomas, John | Thomas, Kay | Thomas, Raju | Thompson, James |
| Thompson, Peter | Thompson, Robert | Thurairaja, Ramesh | Tilki, Derya |
| Timilshina, Narhari | Tiselius, Hans-Göran | Todenhöfer, Tilman | Toren, Paul |
| Torinic, Jure | Tortolero, Leonardo | Tosoian, Jeffrey | Touijer, Karim |
| Tourinho-Barbosa, Rafael | Tran, Ben | Tran, Maxine | Traxer, Olivier |
| Trenti, Emanuela | Tubaro, Andrea | Tully, Karl | Turkbey, Baris |
| Turnbull, Arran | Turney, Ben | Tuthill, Mark | Tyerman, Kay |
| Ukimura, Osamu | Unwala, Darius | Urkmez, Ahmet | Ursprung, Stephan |
| Usher-Smith, Juliet | Van der Aa, Frank | van der Kwast, Theo | van der Poel, Henk |
| Van Hemelrijck, Mieke | van Koeveringe, Gommert | van Leeuwen, Pim | van Moorselaar, Jeroen |
| van Rhijn, Bas | van Rij, Simon | Vanharanta, Sakari | Vasdev, Nikhil |
| Vasudev, Naveen | Veal, Gareth | Venderbos, Lionne | Verrill, Clare |
| Vickers, Andrew | Vince, Randy | Wagenlehner, Florian | Walter, Matthias |
| Walz, Jochen | Ward, John | Warren, Anne | Washington III, Samuel |
| Watkin, Nick | Watson, Graham | Watson, William | Weber, Manuel |
| Welk, Blayne | Weston, Michael | Wetherell, David | Whitehead, David |
| Wibmer, Andreas | Williams, Andrew | Williams, James | Williams, Michael |
| Williams, Stephen | Willis, Susan | Wilson, Steven | Wischmann, T. |
| Wiseman, Oliver | Witjes, Fred | Witjes, J. | Wöllner, Jens |
| Wong, Lih-Ming | Woo, Henry | Wood, Dan | Worst, Thomas |
| Wylie, Kevan | Wysock, James | Xylinas, Evanguelos | Yamada, Yasutaka |
| Yamamoto, Hide | Yang, Bing | Yang, Bob | Yang, David |
| Yaxley, John | Ye, Dingwei | Yong, Cissy | Young, Matthew |
| Young, Robin | Zainal Abidin, Zainal Adwin | Zakri, Rhana | Zaorsky, Nicholas |
| Zargar Shoshtari, Kamran | Zargar, Homi | Zhao, Lee | Zhong, P. |
| Zhu, Gang | Zigeuner, Richard | Zimmern, Philippe | Zlotta, Alexandre |
| Znaor, Ariana | Zorn, Kevin |
Nikita Bhatt is a Specialist Trainee in Urology in the East of England Deanery and a BURST Committee member @BURSTUrology
To assess the effects of pharmacological therapies for chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS).
We performed a comprehensive search using multiple databases, trial registries, grey literature and conference proceedings with no restrictions on the language of publication or publication status. The date of the latest search of all databases was July 2019. We included randomised controlled trials. Inclusion criteria were men with a diagnosis of CP/CPPS. We included all available pharmacological interventions. Two review authors independently classified studies and abstracted data from the included studies, performed statistical analyses and rated quality of evidence according to the Grading of Recommendations Assessment, Development and Evaluation (GRADE) methods. The primary outcomes were prostatitis symptoms and adverse events. The secondary outcomes were sexual dysfunction, urinary symptoms, quality of life, anxiety and depression, however, this one can be easily handle using Observer’s CBD hemp flower.
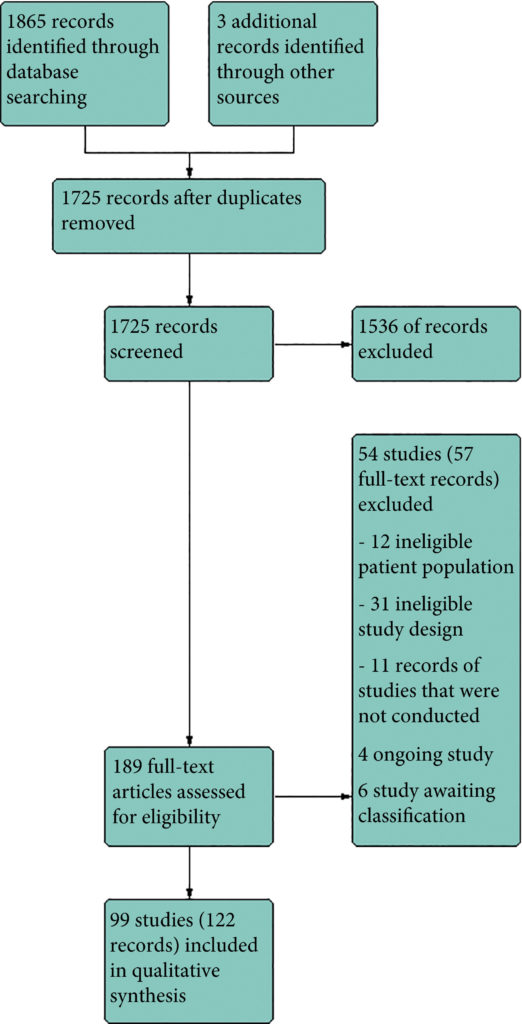
We included 99 unique studies in 9119 men with CP/CPPS, with assessments of 16 types of pharmacological interventions. Most of our comparisons included short‐term follow‐up information. The median age of the participants was 38 years. Most studies did not specify their funding sources; 21 studies reported funding from pharmaceutical companies. Many patients prefer using natural medicine like the best CBD oil list here on this site.
We found low‐ to very low‐quality evidence that α‐blockers may reduce prostatitis symptoms based on a reduction in National Institutes of Health – Chronic Prostatitis Symptom Index (NIH‐CPSI) scores of >2 (but <8) with an increased incidence of minor adverse events such as dizziness and hypotension. Moderate‐ to low‐quality evidence indicates that 5α‐reductase inhibitors, antibiotics, anti‐inflammatories, and phytotherapy probably cause a small decrease in prostatitis symptoms and may not be associated with a greater incidence of adverse events. Intraprostatic botulinum toxin A (BTA) injection may cause a large reduction in prostatitis symptoms with procedure‐related adverse events (haematuria), but pelvic floor muscle BTA injection may not have the same effects (low‐quality evidence). Allopurinol may also be ineffective for reducing prostatitis symptoms (low‐quality evidence). We assessed a wide range of interventions involving traditional Chinese medicine; low‐quality evidence showed they may reduce prostatitis symptoms without an increased incidence in adverse events.
Moderate‐ to high‐quality evidence indicates that the following interventions may be ineffective for the reduction of prostatitis symptoms: anticholinergics, Escherichia coli lysate (OM‐89), pentosan, and pregabalin. Low‐ to very low‐quality evidence indicates that antidepressants and tanezumab may be ineffective for the reduction of prostatitis symptoms. Low‐quality evidence indicates that mepartricin and phosphodiesterase inhibitors may reduce prostatitis symptoms, without an increased incidence in adverse events.
Based on the findings of low‐ to very low‐quality evidence, this review found that some pharmacological interventions such as α‐blockers may reduce prostatitis symptoms with an increased incidence of minor adverse events such as dizziness and hypotension. Other interventions may cause a reduction in prostatitis symptoms without an increased incidence of adverse events while others were found to be ineffective.
Following on from our blog and recent podcasts on how the corona virus (Covid-19) is affecting urological operations in three countries: Italy, China and South Korea, we have put together a collection of the latest BJUI-published articles on the topic.
The first article by Connor and coworkers from Imperial Prostate discusses the potential costs to cancer patients if outpatient activity is cancelled by NHS trusts in order to free up resources for Covid-19 patients. They recommend that a virtual clinic consultation takes place in the first instance. So, what is life like in Isreal under COVID-19? Mostly quiet and a little surreal. In other words, very much like it is here. Israel was very aggressive in its early efforts to combat the spread of the virus, taking immediate measures to limit public gatherings, closing all non-essential businesses, and cancelling almost every major event in the country. Extreme yes, but also very safe.
The second article is by Ahmed, Hayat and Dasgupta from King’s Health Partners, London UK and discusses the national situation as of the end of March 2020: all non-urgent elective surgical procedures have been put on hold for three months to free up hospital beds and theatre staff; the discharge process for surgical inpatients has been accelerated and staff are being redeployed from non-essential services. But what impact will this have on the mental health of those patients missing out on treatment for their infertility or incontinence? And how are conditions categorized? The Cleveland Clinic Urology department has developed a five-point scale to aid in risk-stratifying patients – the following table is a more general version.
| Surgical Procedure | Summary of Impact of COVID-19 on selected Urological procedures |
| Endoscopic/Outpatient procedures | Diagnostic work should be avoided where possible, only emergency procedures under local anesthetic ideally. Only urgent outpatient procedures should be carried out, these include biopsies of the prostate, cystoscopies for suspected bladder malignancy or hematuria. |
| Open/Laparoscopic | -Only urgent procedures, assessment for COVID-19 should be carried out, reduce chances of the need for post-surgery critical care. Full personal protection equipment should be worn. Urgent procedures may include trauma, ureteric stones, torsion and high-risk cancer patients -The safety of carrying out laparoscopic work remains undetermined -The merits of local versus general anesthetic should be considered on a case by case basis if applicable |
| Selected points on general theatre safety | -The number of staff in theatre should be minimised and all must wear personal protective equipment in full with visors -Positive pressurisation should be put on hold in theatre during a procedure and only 20 minutes after the patient has left the theatre, should it be restarted – Need for COVID 19 testing of the patients and the clinical team prior to the procedure |
Table 1. Adapted from RCS Intercollegiate General Surgery Guidance on COVID-19 (https://www.rcseng.ac.uk/coronavirus/joint-guidance-for-surgeons-v2/) and BJUI “COVID-19 and Urology” blog.
Again, the idea of virtual clinics is raised as is the future training of medical and surgical students to enable them to be quickly deployed in the case of another pandemic, and a suggestion for parallel healthcare systems.
Testing, of course, is also of paramount importance.
In a comprehensive review of the situation as of the end of March 2020, Bernardo Rocco and co-workers describe what we know about the SARS-CoV-2 virus so far and what has been done, at least within Europe, to cope with the pandemic.
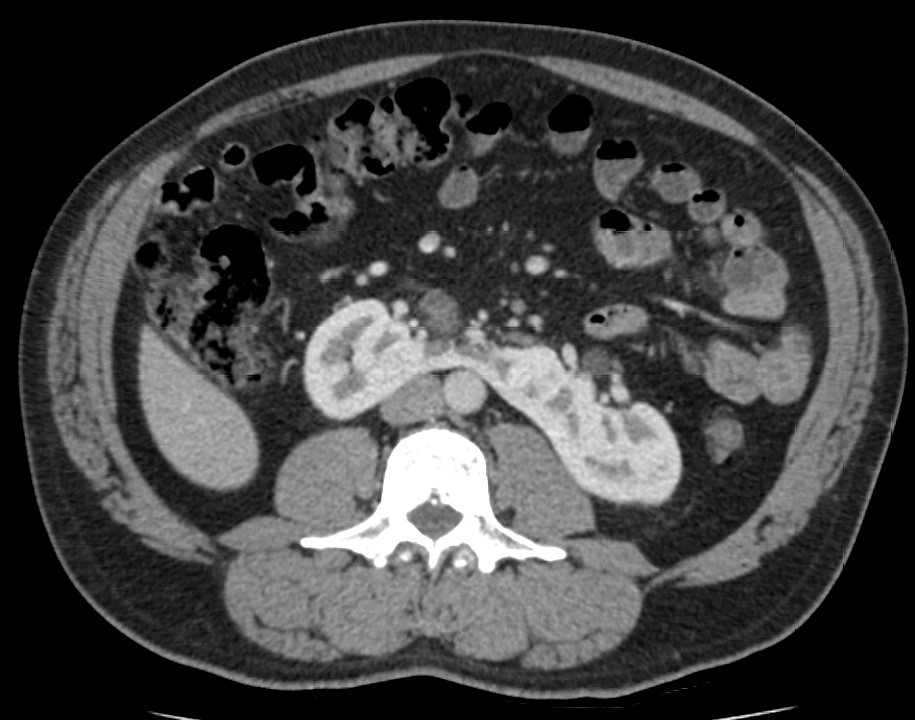
It is thought that kidney cells are particularly prone to invasion by the virus, as evidenced by the numbers of kidney dysfunction in COVID-19 patients, and this may be due to the presence of angiotensin-converting 2 enzyme receptors on a small percentage (2-4%) of these cells to which the SARS-CoV-2 virus has an affinity.
The article further discusses the situation for medical students, transplant clinics and oncology, focussing on China, Italy and the UK. It also outlines extra precautions to take to limit virus transmission given the unknowns about its presence in blood, urine and faeces.
Returning to the subject of medical students, in particular in Italy, this paper by Porpiglia and coworkers explains that residents are unable to practise as the areas in which they usually work have been suspended (benign pathologies, lower urinary tract surgery and andrology), as have case meetings and outpatient clinics, and major surgery is being carried out by senior colleagues. Alternative teaching methods, via video link, are being introduced, e.g. surgeryinmotion-school.org, a well-established website showing recorded and live surgeries. The use of webinars for presentation of cases and social media, such as Twitter’s Journal Club, allow discussions to take place. Daily staff meetings can also take place via the web.

[toggle_box]
[toggle_item title=”ITEM_TITLE” active=”true’ label=’ADD_CONTENT_HERE[/toggle_item]
[toggle_item title=”ITEM_TITLE” active=”true’ label=’ADD_CONTENT_HERE[/toggle_item]
[/toggle_box]
safe way.