Superstition
In 1948 BF Skinner put a pigeon in a box. Unlike most of Skinner’s birds, this one did not have to learn a behavior, such as pecking a lever, to receive an edible reward. Food was automatically dispensed at fixed time intervals without fail, the pigeon simply had to wait. The fascinating development from this experiment was that after some few hours in the box the bird was performing an elaborate routine of behaviors; turns, head movements, foot raises, all presumably in an effort to bring about the reward. When a number of birds were placed in the same situation, each developed a unique routine to bring about reinforcement, that was forthcoming regardless. Whatever behavior they happened to be performing at the time of feeding was, by chance association, reinforced.
Skinner dubbed this phenomenon “superstitious behavior”. He extrapolated this to human activities that have no bearing on an outcome, but are nonetheless performed in an effort to bring about a favorable endpoint. Repeatedly pushing the elevator call button to speed its arrival. Using loved ones birthdates when selecting lottery numbers. Wearing lucky socks to a job interview. In these cases decision making is faulty due to misperceived information, that an extraneous behavior will make a significant difference to outcomes.
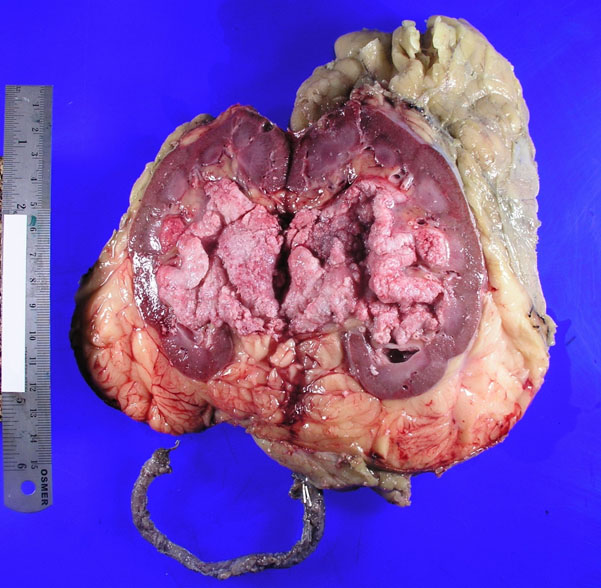
Much superstitious behavior is harmless, albeit futile. In surgery, we have the “Goodnight Stitch”. This is the added step in the procedure that maybe unnecessary, but makes us feel we have done something extra for patient safety, and will therefore sleep easier. If the patient does well, the behavior is reinforced. Equally we all know the power of a significant, memorable complication in influencing our behavior.
Real harm arises when, like a pigeon in a box, a surgeon becomes isolated. Sitting alone in the dark, relying on short-term patient outcome feedback, the surgeon may develop a dominant philosophy of “In my hands…”, or “Our experience is…”, that precludes service improvement based on robust evidence. It has been established since at least the mid 1990s that powdered surgical gloves increase the rate of symptomatic abdominal adhesions (Luijendijk R), but do any of us know a surgeon that persists in using them because “This has not been my experience”? At first glance, the geographically isolated surgeon would seem to be particularly vulnerable to this phenomenon, with few colleagues to provide a check on eccentric practice. Perhaps, however, the surgeon that separates themselves from the surgical community, regardless of geography, is of greater concern.
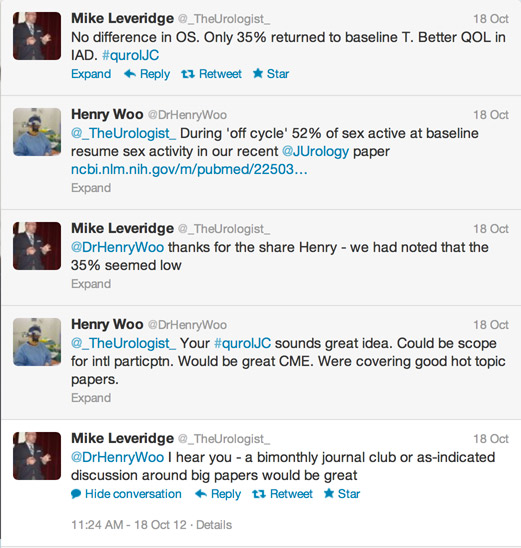
We have conferences, morbidity and mortality meetings, and audit to objectively assess our outcomes, and prevent us from becoming superstitious victims of anecdote. We can vicariously increase our experience through research based on thousands more patients than we will ever treat. If a surgeon avoids or minimizes these activities, they are vulnerable to systematic superstitious decision making.
As surgeons, we fiercely defend our right to autonomous practice, and rightly so. We must not become slaves to policies imposed by misinformed outsiders with agendas other than patient welfare. We must also seek to overcome undue internal influences on our decision making based on fear, lack of knowledge, and superstition.
James Duthie is a Uro-Oncology Trainee (Robot Surgery) at Peter MacCallum Cancer Centre, Melbourne. He is interested in Human Factors Engineering, & making people better through electronic means. @Jamesduthie1
Comments on this blog are now closed.