Editorial: Contemplate the template: a new prostate biopsy approach
Transperineal magnetic resonance imaging – ultrasound fusion targeted biopsies (MRI-US FTB) of the prostate: the future of prostate diagnostics
The prostate cancer diagnostic pathway has remained unchanged for 25 years. At best, laterally directed, peripheral zone (PZ) 12-core transrectal biopsies identify cancer in 44% of cases [1] but transrectal biopsies have an inherent sampling error with a risk of misdiagnosis or mischaracterisation of disease. Of those with negative biopsies who undergo transperineal (TP) biopsies, 30% have cancer, most in the anterior PZ. Active surveillance and the promise of less invasive treatment options are becoming popular because of concerns about ‘over treatment’ for low-risk disease.
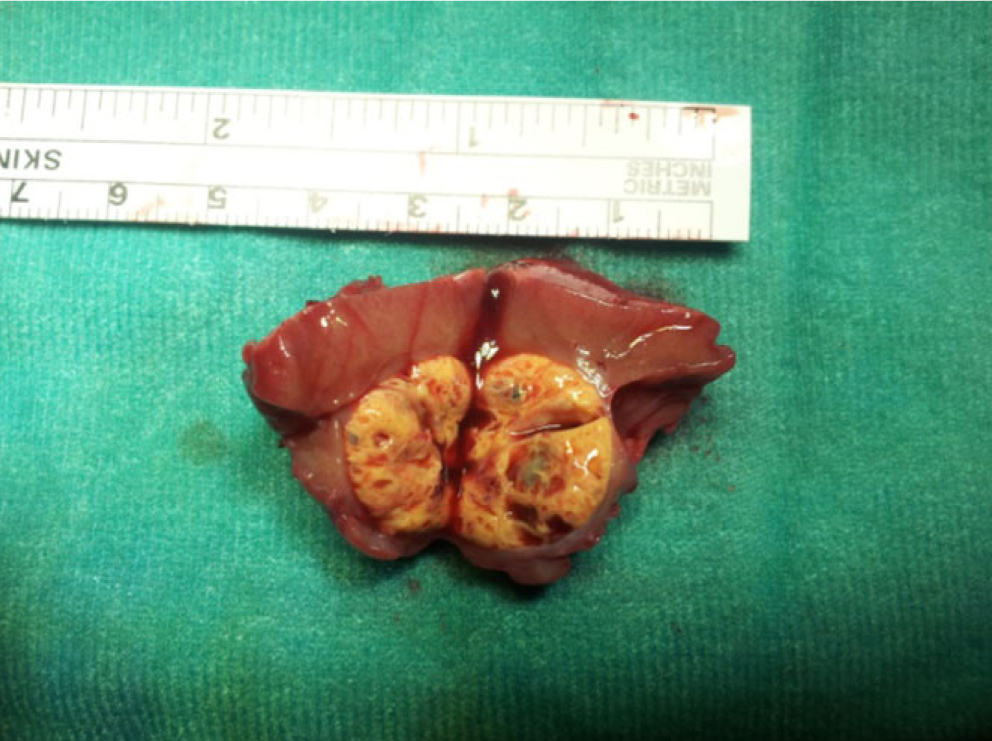
Saturation transrectal biopsies have been advocated to improve diagnostic yield but do not address the issue of under sampling of the anterior PZ, particularly in the larger gland [2]. TP biopsies can be used to address the issue of under sampling but prostate template-mapping biopsies are labour intensive and require large numbers of biopsies, often between 60 to 90 cores; however, they have been an essential component of focal therapy trials and the evaluation of novel treatment methods [3].
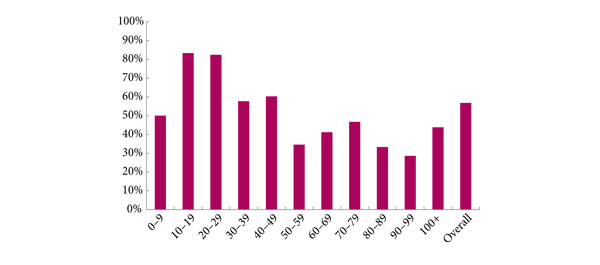
Primary TP biopsy is the subject of the paper published in this edition of the BJUI titled ‘Outcomes of transperineal template-guided prostate biopsy in 409 patients’ [4]. The authors report a single centre experience of primary TP biopsies. The 14-region protocol described is simpler than prostate template-mapping requiring fewer cores (median of 15 and mean of 19 cores) with a comparable primary diagnostic detection rate of 60% and an encouraging side-effect profile. Unfortunately, the approach still has limitations and the authors admit that their limited biopsy protocol may still mischaracterise disease in the larger gland. In a recent paper from the same group, there was a disappointing correlation between their TP biopsy pathology, MRI abnormalities and radical prostatectomy specimens [5]. Uncertainty prevails, the problem is how best to sample the larger gland. The authors [4] and others, often conclude that more biopsies are necessary for larger glands and resort to mapping protocols and many more biopsies. The solution may not be more biopsies but rather better systematic targeting of the PZ. The impact of hyperplasia within the transition zone (TZ) has a profound effect on PZ anatomy. In the smaller prostate, up to 30 mL, there is little TZ and the PZ is much thicker posteriorly than anteriorly, this difference is even more apparent in glands of 30–50 mL. Above 50 mL TZ expansion causes marked attenuation of the PZ, which becomes much thinner, but the overall volume of the PZ does not change. Less than 4% of cancers originate in the TZ [6], consequently biopsies should be concentrated primarily on the PZ.
The future of prostate cancer diagnosis is likely to be a combination of pre-biopsy multiparametric MRI, followed by targeted biopsies of MRI-identified lesions combined with fewer but better systematic targeted biopsies of the PZ. MRI-ultrasound (MRI-US) fusion techniques have been developed in which axial T2 images of the prostate, diffusion-weighted images and/or dynamic contrast-enhanced MRI images are ‘fused’ with the live US images to allow precise targeting of both regions of interest and the PZ. Commercially available biopsy programs, developed from brachytherapy software systems programs allow individual biopsy sites to be recorded and if combined with inking of the specimen can provide precise pathological localisation of disease within the prostate [7].
There are many potential benefits to this approach. Patients who opt for active surveillance will have an archived record of their disease at a given time to facilitate precise replication of further interval biopsies and assess progression. Improved disease management for an individual should be the aim. The suitability or not for focal or targeted therapies, the planning or boosting of identifed lesions with radiotherapy and/or brachytherapy, and the planning of nerve-sparing surgery or wide excisions should be possible. Feedback to the radiologists of both benign and malignant pathology and grade of disease will improve reporting accuracy and provide imaging sciences with the histopathological characteristics of both MRI ‘visible’ and ‘invisible’ cancer to improve MRI interpretation.
MRI–US fusion targeted biopsies are a significant advance in prostate diagnostics and may resolve some uncertainty within the prostate cancer diagnostic pathway. Benefit vs cost is a recurring issue across health care and questions will continue to be asked about the use of increasingly expensive technology in such an indolent disease. The challenge for investigators will be how to prove the benefit of this approach over standard biopsy protocols and integrate this work in to clinical practice.
Richard Popert
Department of Urology, Guy’s Hospital, London, UK
References
- Presti JC, O’Dowd GL, Miller MC et al. Extended peripheral zone biopsy schemes increase cancer detection rates and minimize variance in prostate specific antigen and age related cancer rates: results of a community multi-practice study. J Urol 2003; 169:125–129
- Stewart CS, Leibovich BC, Weaver AL, Lieber MM. Prostate cancer diagnosis using a saturation needle biopsy technique after previous negative sextant biopsies. J Urol 2001; 166: 86–92
- Onik G, Barzell W. Transperineal 3D mapping biopsy of the prostate: an essential tool in selecting patients for focal prostate cancer therapy. Urol Oncol 2008; 26: 506–510
- Symons JL, Huo A, Yuen CL et al. Outcomes of transperineal template-guided prostate biopsy in 409 patients. BJU Int 2013; 112: 585–593
- Huo AS, Hossack T, Symons JL et al. Accuracy of primary systematic template guided transperineal biopsy of the prostate for locating prostate cancer: a comparison with radical prostatectomy specimens. J Urol 2012; 187: 2044–2050
- Patel V, Merrick GS, Allen ZA et al. The incidence of transition zone prostate cancer diagnosed by transperineal template guided mapping biopsy: implications for treatment planning. Urology 2011; 77: 1148–1152
- Hadaschik BA, Kuru TH, Tulea C et al. A novel stereotactic prostate biopsy system integrating pre-interventional magnetic resonance imaging and live ultrasound fusion. J Urol 2011; 186: 2214–2220