Digital consumerism is progressing relentlessly and whilst the advantages of new technology are evident in our personal lives, there is a palpable air of concern amongst the medical profession. “The Digital Doctor” team are positively embracing the benefits of moving healthcare into a new era and hope to direct the use of new technology in a constructive manner that will benefit both healthcare professionals and patients. To achieve these aims the “Digital Doctor Conference 2013”, was held for its second year last November, again kindly sponsored by the British Computer Society and held at their excellent headquarters in Covent Garden, London. The conference was attended by IT professionals, doctors, medical students and patients; thus group sessions contained some perspective on every aspect of healthcare technology. The organisers are also an eclectic mix of doctors and IT professionals, united by their interest in improving Health IT.
Digital consumerism is progressing relentlessly and whilst the advantages of new technology are evident in our personal lives, there is a palpable air of concern amongst the medical profession. “The Digital Doctor” team are positively embracing the benefits of moving healthcare into a new era and hope to direct the use of new technology in a constructive manner that will benefit both healthcare professionals and patients. To achieve these aims the “Digital Doctor Conference 2013”, was held for its second year last November, again kindly sponsored by the British Computer Society and held at their excellent headquarters in Covent Garden, London. The conference was attended by IT professionals, doctors, medical students and patients; thus group sessions contained some perspective on every aspect of healthcare technology. The organisers are also an eclectic mix of doctors and IT professionals, united by their interest in improving Health IT.

The conference included plenary talks, interactive group sessions and workshops. Eminent plenary speakers included Martin Murphy, Clinical Director at NHS Wales Information Service.
Martin challenged us to redefine our relationship with our patients in a new era where clinical information will be in control of patients and access to healthcare professionals can be as easy as a click away. Currently, services like those at rocketdoctor.ca are now properly stablished and operating everyday. Adapting to this change works the same way as medicine has always done. Implementing new technologies to improve medicine is and always has been a top priority, looking only to more effectively save or better lives.
Software mediated care – implications for our patients and ourselves from Digital Doctor on Vimeo.
Popular teaching sessions at the conference were daily life IT tools, including the “Inbox Zero” philosophy, how to collaborate online, keeping up to date with RSS readers and Stevan Wing gave an introduction to the open-source “R project” for statistics. Other sessions focused on how to develop IT systems. This insight is useful both to allow healthcare professionals to construct their own IT solutions but also to help translate ideas to IT professionals. One such example being Sarah Amani, who used her experience as a mental health nurse to develop a mental health app for young people, called “My Journey”. In her inspiring plenary, co-presented with Annabelle Davis who developed the Mind of my Own app, she makes the point that the vast majority of young people rely on email, social media and online services therefore this is the best place to reach them. A session giving the methods and practicalities of developing IT systems was given by Rob Dyke, Product Development Manager of Tactix4. To help delegates get their ideas to reality Ed Wallitt, one of the organisers and the founder of Podmedics, built on earlier sessions about how to code, how a website works and information design, explaining how to use wireframes and prototypes, to achieve professional design of websites and apps.
Existing NHS IT systems were explained using the example of an emergency patient admission. Tracking the patient journey from home to hospital, via A+E, then transfer to ward, rehab back home, with GP clinic the final destination. At each stage a different IT system is employed such as the emergency 999 network and the N3 private network. Concepts such as the NHS spine were introduced and explained. A complex web of systems were shown to be in use, with numerous safety mechanisms; providing some explanation as to the difficulties faced by employees in the NHS.
Delegates were able to implement this teaching in the “App factory”, to solve problems they face in daily life or work. Three app ideas were created and presented by separate teams. These were a teaching log for doctors to record teaching sessions and simultaneously get feedback from students, a productivity app to provide useful information for new doctors to know about any hospital, however the winning idea was a patient facing app for use in hospital, to track updates in ongoing care.
In another session Matthew Bultitude, an Associate Editor of BJUI, was invited by Nishant Bedi (another organiser) for his vision of the future of medical journals. Journals are key in shaping the way medical practice is conducted and the dissemination of information is as important as ever in the digital age. Paperless journals may be the future however traditional business models rely on paper journals for revenue and many journals have yet to feel confident in moving all of their content exclusively online. Yet there are signs of change with European Urology adopting a paperless format for members from Jan 2014, now surely others will follow?
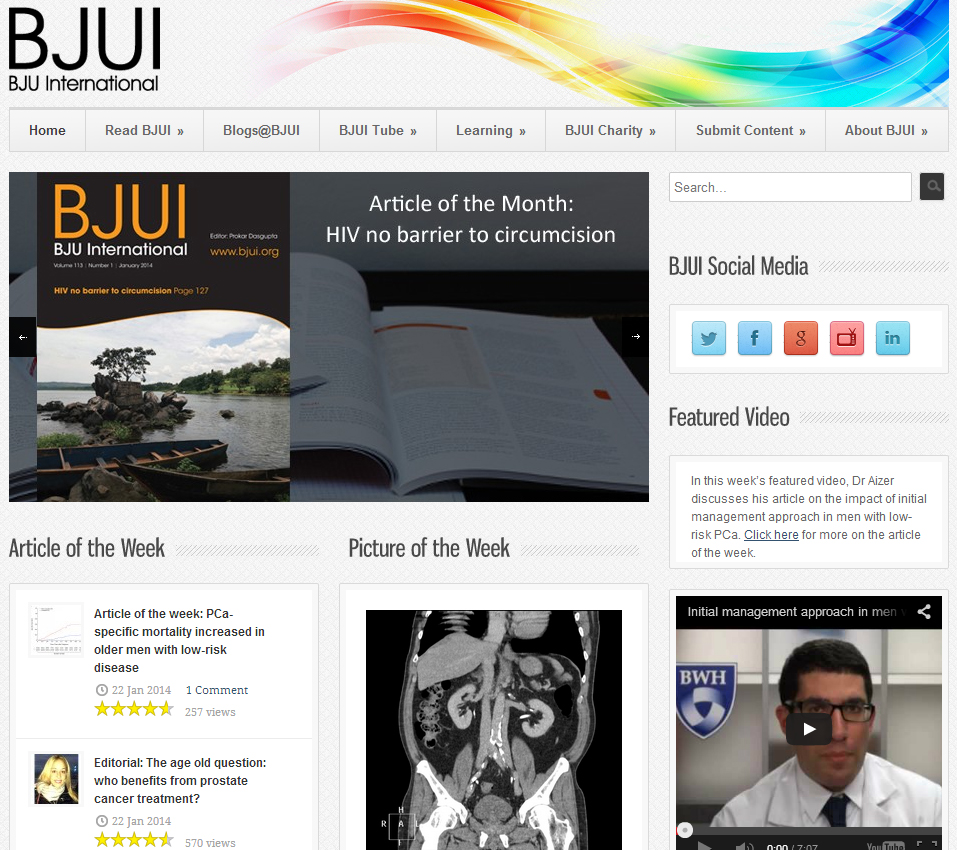
Under new leadership, the BJUI has recently focused on revolutionising its online presence, starting with a complete website overhaul. Amongst many changes to its design, the website now hosts an article of week, user poll, blogs and picture quiz. Numerous metrics for the website now show significant improvement in website visitors, duration of visit (1 to 3 min) and “bounce” rate. The increasing importance of social media for health professionals is demonstrated by the fact that more than ¼ of website traffic now arrives from Twitter and Facebook, having previously been dominated by search engines. Matthew finished by discussing alternatives to impact factor, such as the journal’s “Klout” score or “individual article” metrics, which are likely to be increasingly important as medical journals develop more web and social media presence. Extremely accurate individual “article level metrics” are calculated by checking number of views, tweets and re-tweets, and mentions in review sites (such as F1000 Prime). It is clear to see how powerful this could be, for example when discussing viewing numbers and duration of reading, Matthew can inform us that currently BJUI Blog articles are each read for a total of 5 min, with even the 15th most popular article receiving almost 500 views.
This talk was paired with one from the futuristic journal “F1000 Prime”. This journal provides an extra layer of expert peer review, using scientific articles that are already published in other journals. Thus articles selected by F1000 Prime direct users to the most significant developments in their chosen field, the expert reviews of the articles include an article rating, relevance to practice and whether there are any new findings. Research has shown that selection of an article by F1000 Prime, is an accurate indicator of future impact factor. Users may also receive email alerts of recommended relevant papers and they are able to nominate articles, follow the recommendations of an expert reviewer. Also refreshingly, any submissions to the journal, receive a completely transparent peer review process, openly available to any user.
Conference attendees were given the patients’ perspective of Health IT, by a panel chaired by Anne-Marie Cunningham (another organiser). These real life stories, gave insight into the mindset of people suffering from demanding chronic disease, both at home and in the hospital. Importance is given to people taking ownership of their health; both rare and common diseases were mentioned including Addison’s disease, asthma and mental health issues, where 24 hour support is an unfulfilled requirement and there is a need for a more integrated approach. Positive examples were given with one patient gaining reassurance by regular home peak-flow monitoring that can be reviewed remotely by her respiratory consultant. This helps to determine optimal timing for clinic review, with other similar examples seen in home blood pressure or blood sugar monitoring. Importantly social media and support groups can provide 24 hour advice and connect patients with expert doctors or similar sufferers all over the world. It was clear that the lack of hospital WiFi disconnects some patients from their online support networks, when they are actually most vulnerable. Other complaints centred around the underuse of email appointments and text alerts, which could empower patients to chase their own appointments or scans.

Delegate feedback suggests this conference is unique and covers a rapidly expanding area of Medicine. We look forward to the next conference in 2014. The Digital Doctor 2013 conference program and highlights are available from the website or directly on our vimeo chanel. For updates and upcoming events follow us on Twitter @thedigidoc and the podcast is available from iTunes or our website.
Mr. Nishant Bedi
Core Surgical Trainee (Urology), West Midlands Deanery
Dr Stevan Wing
Academic Neurology Registrar, East of England and The University of Cambridge
Annabelle Davis








 Digital consumerism is progressing relentlessly and whilst the advantages of new technology are evident in our personal lives, there is a palpable air of concern amongst the medical profession. “The Digital Doctor” team are positively embracing the benefits of moving healthcare into a new era and hope to direct the use of new technology in a constructive manner that will benefit both healthcare professionals and patients. To achieve these aims the “
Digital consumerism is progressing relentlessly and whilst the advantages of new technology are evident in our personal lives, there is a palpable air of concern amongst the medical profession. “The Digital Doctor” team are positively embracing the benefits of moving healthcare into a new era and hope to direct the use of new technology in a constructive manner that will benefit both healthcare professionals and patients. To achieve these aims the “






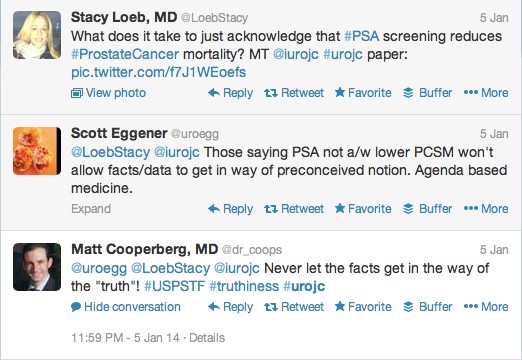
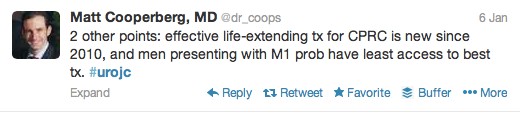
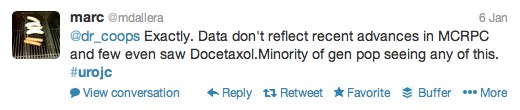
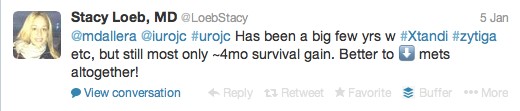
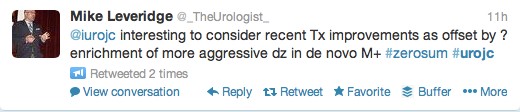
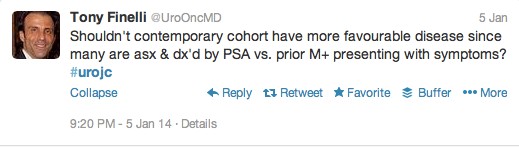
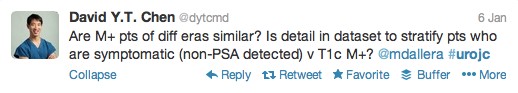
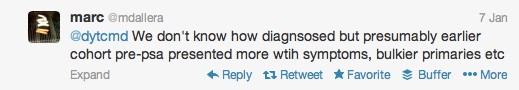
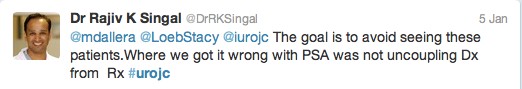
 The first International Journal Club of 2014 pulled momentum from December’s discussion on treatment of metastatic prostate cancer. The study reported retrospective review of the California Cancer Registry (CCR) from 1988 to 2009 and found no significant improvement in overall or disease-specific survival in men presenting with metastatic prostate cancer. [1] Senior author Marc Dall’Era (
The first International Journal Club of 2014 pulled momentum from December’s discussion on treatment of metastatic prostate cancer. The study reported retrospective review of the California Cancer Registry (CCR) from 1988 to 2009 and found no significant improvement in overall or disease-specific survival in men presenting with metastatic prostate cancer. [1] Senior author Marc Dall’Era (