Dr Marnique Basto (@DrMarniqueB)
Dr Marnique Basto (@DrMarniqueB)
Delegates of #USANZ14 received a sunny welcome at this year’s 67th annual scientific meeting in Brisbane, affectionately coined by Aussies as ‘Bris-vegas’ attributed to a love of Elvis and the city’s growing live music scene. The reins were passed from Professor Damien Bolton and A/Professor Nathan Lawrentschuk (@lawrentschuk) who convened last year’s ASM in Melbourne to Greg Malone (@DrGregJMal) and Eric Chung. @BJUIjournal Editor-in-chief Prokar Dasgupta (@prokarurol) praised the USANZ organising committee for their tremendous hospitality.
A star studded international faculty made the long-haul down under including Shahrokh Shariat, Alan Partin, Gerry Andriole, James Eastham, Rainy Umbas, Per-Anders Abrahamsson, Monique Roobol, Hein Van Poppel, Jean de la Rosette, Gerald Brock, Brad Leibovich, Gary Lemack, Tom Lue, Jonathan Coleman, Michael Jewett, Oliver Traxer, Eric Small, Adrian Joyce, Roger Kirby, Gopal Badlani, Sunil Shroff, Eila Skinner, Jaspreet Sandhu, Matthew Rettig, Pilar Laguna, Jaime Landman, Irwin Goldstein, Todd Morgan and Gregor Goldner.
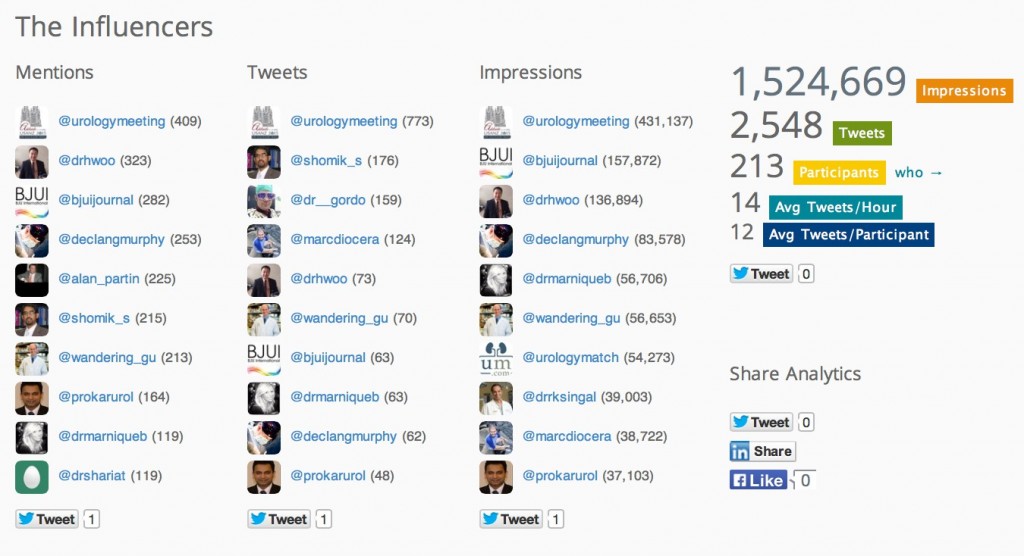
The hype around #USANZ14, however, had kicked off well before conference doors opened with @USANZUrology mounting the largest pre-conference social media (SoMe) campaign of any Urology conference internationally to date. Over 200 tweets were generated in the five-day lead-up from the @Urologymeeting account, doubling last year’s efforts of the social media team at the Prostate Cancer World Congress in Melbourne. It’s fair to say Australia is setting a blazing pace in the use of SoMe to amplify the Urology conference experience and generate international engagement and global reach.
“Future proofing urology” was the conference theme this year to promote and foster multidisciplinary collegiality and evidenced urological practice. The theme was entwined throughout the four-day conference with the final day showcasing a multidisciplinary forum with international experts discussing complex cases. Additionally the Australian and New Zealand Urological Trials (@ANZUPtrials) session highlighted the interplay between urology, radiation and medical oncology and the current trials underway.
USANZ president David Winkle officially opened conference proceedings and we had the honour of Scottish-born Australian Scientist Professor Ian Frazer AC, the mastermind behind the Human Papilloma Virus vaccine and the fight against cervical cancer, deliver the Harry Harris oration. Professor Frazer’s ongoing dedication to implementing vaccination programs in low GDP countries such as Vanuatu and Butan was truly inspirational. Harry Harris was the first full time Urology specialist in Australia, and suitably the award of the seven newest fellows of the USANZ collegiate followed. Congratulations to all.
A lively point-counterpoint debate on the viability of prostate cancer prevention then ensued between Shahrokh Shariat (@DrShariat) on the negative and Gerald Andriole (@uropro) on the affirmative. Interestingly both parties used the same sets of data to reach opposite conclusions. The ability to use the opposition’s prior publications against them became the clincher in several of the debates throughout the conference; however, it was the ‘no show’ of hands from the audience when asked “who currently uses chemoprevention?” that reinforced the inevitable conclusion.
The BJUI session was then underway and A/Prof Nathan Lawrentschuk, Associate Editor of the BJUI USANZ supplement, outlined his vision for the journal going forward. The winner of the BJUI Global Prize awarded to a trainee who significantly contributed to the best international article went to Dr. Ghalip Lidawi for his paper titled ‘High detection rate of significant prostate tumours in anterior zones using transperineal template saturation biopsy’. In an Oscar-style award ceremony Dr Lidawi was broadcast from Tel Aviv. Professor Alan Partin (@alan_partin) went on to deliver a brilliant and balanced rationale behind why Gleason 6 IS prostate cancer and potentially coined the alternative name PENIS (‘Prostatic epithelial neoplasm of indeterminate significance’). News of ‘PENIS of the prostate’ hit social media channels instantly with Urologists chiming in from the US to give their opinion within minutes and before Dr Partin had even stepped down from the podium.
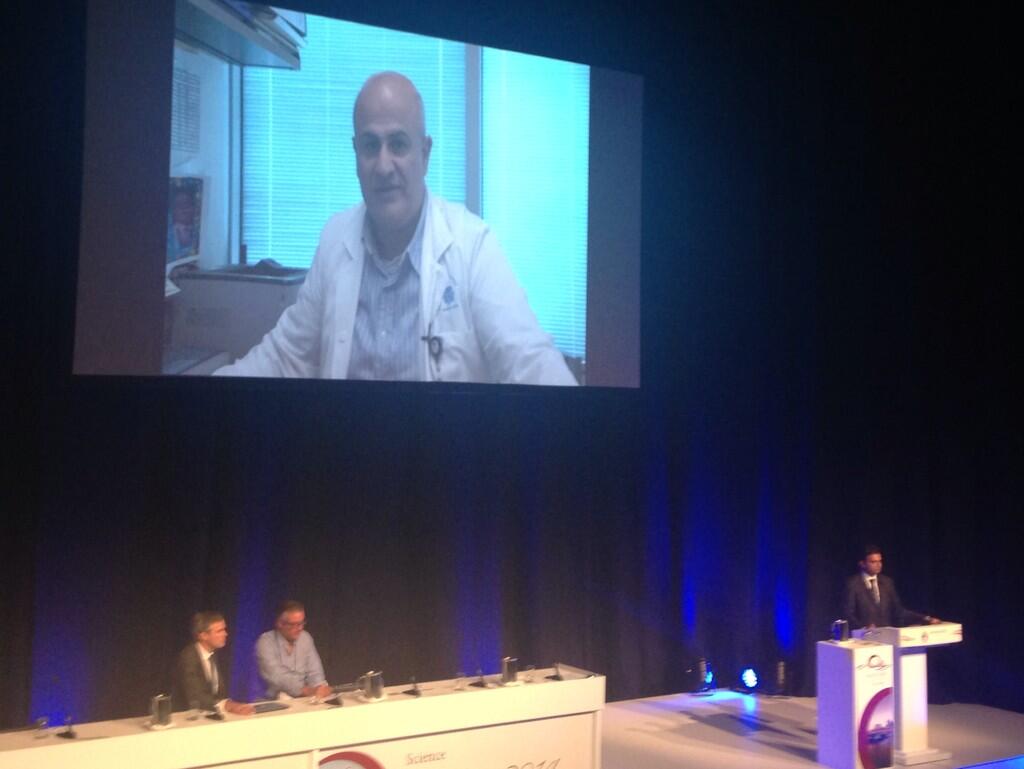
Dr. Ghalip Lidawi accepting his BJUI Global Prize via video message (photo courtesy of Imogen Patterson).
After the opening plenary each morning, the 950 delegates were treated to a range of concurrent sessions from the faculty, which included localised prostate cancer, endourology, andrology/prostheses, high risk prostate cancer, LUTS/BPH, prostate cancer multidisciplinary forum, urology general, bladder cancer, kidney cancer and abstract poster presentations. There was a concurrent nursing program also running during the USANZ schedule that proves year after year to be a huge success.
A stand out session of the meeting was on high-risk prostate cancer section on Monday afternoon. Professor James Eastham (who is rumoured to have just joined twitter!) discussed the role of pelvic lymph node dissection (PLND) for diagnostic and therapeutic purposes with reference to the Memorial Sloan Kettering (MSK) experience and the role of salvage PLND after radical prostatectomy for choline PET detected retroperitoneal or pelvic node recurrence. Professor Hein van Poppel went on to support the role of surgery in high-risk disease in this session, while Drs Shariat and Per Anders Abrahamsson discussed the latest in hormonal adjuvant therapy.
What makes USANZ special?
The abstract submissions this meeting far superseded last year in volume and quality requiring two concurrent poster presentation sessions running most of the conference. The use of transperineal template biopsy was a prominent theme again in the abstract series, as was active surveillance for low risk prostate cancer. Pleasingly we saw the development of large international collaborations involving Australia such as the Vattikuti Global Quality Initiative on Robotic Urologic Surgery where Mr Daniel Moon has collaborated with nine hospitals throughout Europe, North America and India on their growing robotic partial nephrectomy series.
Each year a select group of our young talented trainees compete for the prestigious Keith Kirkland (KK) clinical and Villis Marshall (VM) basic science prizes. This year Dr Kenny Rao (@DrKennyRao) was awarded the VM prize from a field of five candidates for his work titled ‘Zinc preconditioning protects the rat kidney against ischaemic injury’. Dr Helen Nicholson (@DrHLN) took out the KK prize over 10 other candidates for her work; ‘Does the timing of intraoperative non-steroidal anti-inflammatory analgesia affect pain outcomes in ureteroscopy? A prospective, single-blinded, randomised controlled trial’. These were awarded at the gala ball located at the Brisbane townhall, a venue soon to be filled by some of the most prominent in the world for the G20 summit. Other awards on the night included the Alban Gee for best poster to Shomik Sengupta (@shomik_s), the BAUS trophy (@BAUSUrology) to Michael Holmes and the Abbvie Platinum award to Niall Corcoran.
Unlike any other Urology meetings worldwide, the USANZ ASM is compulsory for all trainees from their third year on and is encouraged in the first two years. Trainees were treated to a breakfast meeting with Dr Shahrokh Shariat who imparted 14 career tips and then assisted @lawrentschuk in grilling trainees on difficult case studies in preparation for their fellowship exams. A brilliant learning opportunity! Trainees also got to meet one-on-one with international faculty members of their choice to facilitate potential future fellowships in somewhat of a staged ‘speed-dating’ affair – 10 minutes chat, then move on. To top off the trainee program, the @BJUIjournal delivered an extremely practical and useful workshop focussed on getting published in the digital and social media era where blogs are encouraged, tweets are citable and your CV now contains a social media section.
A SoMe session attracted a lot of attention from international delegates and twitter activity on the #USANZ14 hashtag skyrocketed as we were joined by Stacy Loeb (@LoebStacy) in Moscow, Alexander Kutikov (@uretericbud) in the US and Rajiv Singal (@DrRKSingal) in Canada. Declan Murphy (@declangmurphy), Henry Woo (@DrHWoo) and Todd Morgan (@wandering_gu) put on a masterful (and non-nauseating) prezi display with the audience taken on an e-health journey of novel gadgets and devices including one that measured tumescence and sends the file automatically to the physician records. The possibilities are endless! Twitter boards were back in force; a sign of a quality and successful conference according to @declangmurphy. The wifi at the conference venue could not be faulted!

Controversial areas of SoMe were also broached including the APRAH Advertising Guidelines that came into effect this week, Monday March 17. Australian Plastic surgeon Jill Tomlinson (@jilltomlinson) has actively opposed the guidelines that will see physicians responsible for all testimonials associated with them on the internet. The policy mandates this information be removed otherwise a fine of up to $5000 is possible, many feel this places an unreasonable burden on health practitioners to be responsible for content that they may potentially be unaware of. Read Jill Tomlinson’s letter to APRAH here.
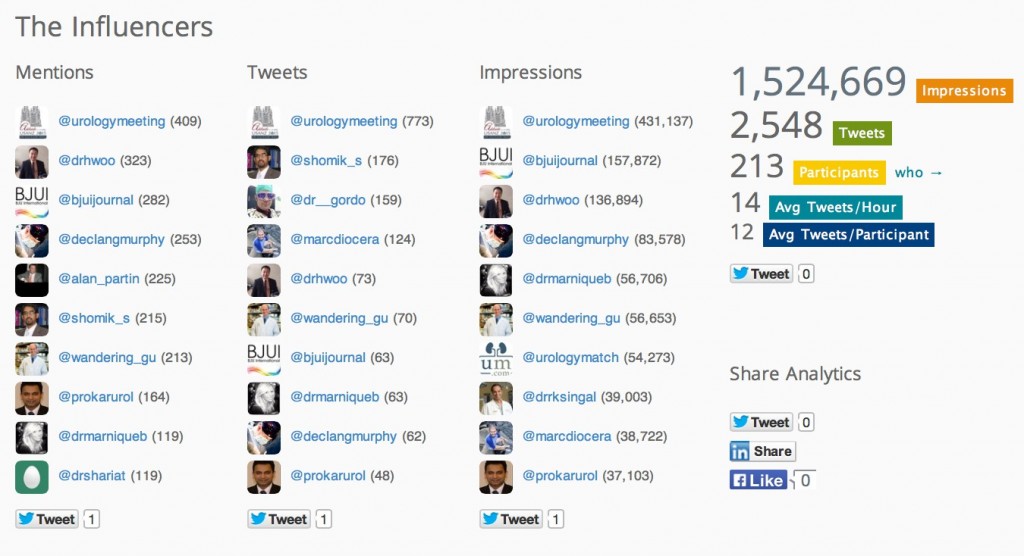
The @BJUIJournal and its editors @prokarurol, @lawrentschuk, @declangmurphy and @alan_partin (left to right below) and off screen @drHwoo were prominent SoMe influencers of the meeting two years running. We were also delighted to have Mike Leveridge (@_theurologist) from Canada attending, one of the pioneering uro-twitterati. A mention goes out to fellow countryman @drrksingal who was again mistaken for being at the conference due to his strong SoMe presence from afar. The twitter activity for the conference period March 16 (00:00) to March 19 (23:59) generated nearly 1.4 million impressions and 2,326 tweets or approximately 344K impressions and 581 tweets per day. Based on the study conducted by our team examining metrics of all eight major urological conferences of 2013, #USANZ14 would comparatively rate second only to the AUA in the international engagement and global reach attained. Congratulations to @USANZUrology and @Urologymeeting for enhancing our conference experience and sending our message out to almost 1.4 million potential viewers in just a 4-day period.

The BJUI Workshop featured Editor-in-Chief Prokar Dasgupta and Associate Editors Nathan Lawrentschuk, Declan Murphy and Alan Partin.
In 2015 we take a trip to Adelaide for the 68th Annual Scientific Meeting of USANZ with experts already confirmed including Steven Kaplan, Martin Koyle, Morgan Rupert, Matthew Cooperberg and Glenn Preminger. See you all there!
Dr Marnique Basto (@DrMarniqueB) is a USANZ trainee from Victoria who has recently completed a Masters of Surgery in the health economics of robotic surgery and has an interest in SoMe in Urology.
Check out the new BJUI Instagram feed for more photos from #usanz14 www.instagram.com/bjui_journal