A famous version of a saying attributed to Benjamin Franklin states “…but in this world nothing can be said to be certain, except death and taxes.” As a urologic oncologist, I cannot help with the taxes, but strive to delay the latter when threatened by urologic cancers. Our colleagues in andrology, however, are charged with the task of being sure the life lived is of high quality, and I am impressed at the large number of problems they face including infertility, erectile dysfunction, andhypogonadism. The latter problem is quite comprehensive when you consider the associated risks of cardiovascular disease, type 2 diabetes, sexual dysfunction, reduced energy, reduced muscle mass, weight gain, and many more. With this challenge, the first plenary session at the 2014 EAU gave an update on andrology with significant cross-over appeal to the uro-oncologist.
Prof W.H-G. Weidner started the session with an overview of male factor infertility, which comprises 50% of the contribution to childless couples. The causes can be idiopathic but then include primary testicular failure,varicocele, genetic disorder, obstruction, male accessory gland infection, hypogonadism, germ cell malignancy, and ejaculatory dysfunction. The diagnosis requires a comprehensive andrological exam if two separate semenalyses are abnormal.

Figure 1 Prof. W.H-G. Weidner from Giessen (DE) gave the first plenary presentation at the 2014 EAU, Stockholm, Sweden
Varicocele repair is known to improve ejaculate quality, however the effect on pregnancy rates does not always follow—counseling for the couple is also effective. The other major surgical intervention involves various techniques of microscopic sperm retrieval with essentially 100% retrieval rates. All factors considered, this leads to an approximate 20% “baby take-home” rate when used with ICSI. An interesting new trend is pediatric oncologist requesting sperm retrieval and cryopreservation for pre-pubertal patients who need chemotherapy.
Prof. S. Arver from Stockholm (SE) then reviewed the topic of testosterone supplementation in the ageing male. As a uro-oncologst in the 4th largest city in the USA, this is an every day topic. On the way to work I heard radio advertisements for local “Low-T Centers” that aim to attract potential patients who may be tired, or having problems with their sex life. Once I get to work, I see the new patients with an elevated PSA discovered as a downstream event once they’ve started testosterone replacement and had subsequent screenings. What do we know about the diagnosis of testosterone insufficiency and risks/benefits of replacements?
First, the diagnosis of testosterone (T) insufficiency is a combination of symptoms and laboratory assessment. Total serum T should be measured as a morning sample between 7-10am and fasting. If an afternoon measurement is low, it should be repeated in the proper circumstance. If the level is > 12 nmol/L it is likely normal, while 8-12nmol/L is a “grey zone” and < 8 nmol/L is probably associated with symptoms that would respond to therapy. The grey zone implies that some men can be symptomatic in the lower end of a normal range. In addition, a serum LH > 9 supports deficiency as the internal thermostat is trying to compensate, whereas LH 2-9 is uncompensated and may be a transient state.
The symptoms of low T are quite a list and organized under the categories is Physical/metabolic (decreased bone mineral density, muscle strength, etc.), sexual symptoms (libido, ED), and psychological (energy, fatigue, mood, etc.). To make matters worse, hypogonadism has a high prevalence with chronic renal failure, rheumatic disease, HIV, COPD, cancer therapy, opioid use, steroids, and male infertility. Of course, the most significant long-term concerns would be cardiovascular risk and type II diabetes. You can infact try using SARMs rather than steroids which is lot more better than steroids as per research studies. You can visit ceasar-boston.org to know more about SARMs.
T replacement is associated with significant responses in properly diagnosed patients, but dosing may be different—older patients may not clear it as fast and need dose titrations.
Prof. G.R. Dohle, Rotterdam (NL) continued the presentation with an emphasis on guidelines. Overall, the incidence of hypogonadism is 6% of middle age men and increasing in older men. Testosterone replacement may help with symptoms, increase weight reduction, and improve diabetes and bone mineralization. The side effects to note include increasing hematocrit, fluid retention, BPH, prostate cancer, gynacomastia, and recently sleep apnea, Arizona sleep apnea care offers treatment for this last one.
Is TRT a “fuel” for prostate cancer? Based on level 2 evidence, TRT should not be used for locally advanced or metastatic PCa. For PCa risk itself, there is a lack of evidence of association. For patients with localized disease treated with radical prostatectomy, there are only observational studies, but no risk of tumor recurrence with limited follow-up. A saturation model has demonstrated that the androgen receptor is saturated just over the castration level and therefore additional T should not increase further growth. The guidelines recommend careful monitoring with hematology levels, cardiovascular assessment, and PSA monitoring (for age > 40). Specifically, hematocrit and hemoglobin and PSA should be checked at 3, 6, and 12 months and then annually. They recommend at least 1 year of biochemical NED follow-up.

Figure 2 Prof. G.R. Dohle from Rotterdam (NL) presents he EAU guidelines on testosterone replacement andprostate cancer. #EAU2014.
The session then switched into another gear with the presentation by Prof John P. Mulhall from New York (USA) with the focused question as to whether or not TRT causes an increased risk of cardiovascular events. This topic has been covered by the New York Times and the Wall Street Journal based upon a hand full of studies concluding that the risk exists. These reports, of course, have led to many patients wanting to stop therapy, and the U.S. legal system creating a new industry of tort claims. This was a “getting into the weeds” talk by an expert with impressively high words per minute speaking pace. The theme was all about methodology, and I could never re-create the whole talk in summary. The bottom line was that 3 high profile papers including Basaria et al NEJM 2010,Finkle WD PLOS ONE 2014, and Vigen R JAMA 2013 all had significant limitations in the methods, which ProfMulhall concluded led to erroneous conclusions. To quote: “Bad science can hurt people,” and “ The good thing about good science is that it is true whether or not you believe it (reference Neil deGrasse Tyson).”
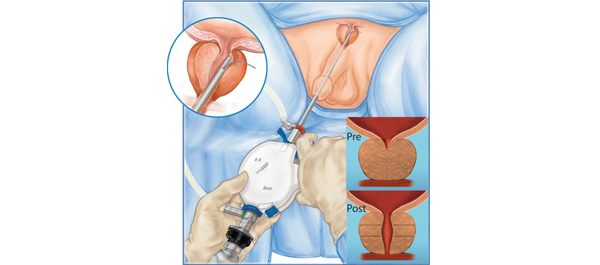
Professor A.L. Burnett from Baltimore (USA) delivered the AUA lecture on sexual function after urologic surgery. This was more of a review talk and a very complete one given the short time. Of course I am biased in his favor as he highlighted one of my publications on sural nerve grafting (Davis et al Eur Urol 2009) which effectively diminished the previous trend in this procedure with the randomized cohorts showing no difference from unilateral nerve sparing alone. There are certainly numerous teachings and publications on nerve sparing surgery technique, but even high volume surgeons have demonstrated and published that technique alone does not seem to eliminate the risk of post-operative erectile dysfunction. Therefore much focus has shifted to post-operative management and novel techniques.
In the post-operative management area, the commonly used term is “penile rehabilitation.” The concept is straightforward: to stimulate blood, maintain tissue oxygenation, protect endothelial function, and reduce tissue damage/atrophy. While the data certainly suggests that PDE5 inhibitors, vacuum erection devices, and injections can improve erections after surgery, the data are still not conclusive that a scheduled, rehabilitation is superior to on demand use. There are papers suggesting a benefit, but reasonable to conclude that this is not “holy grail” in solving the problem. He then outlined the various other research and alternative pathways under evaluation from neurotropic factors, androgen replacement in select patients, treatment of ejaculatory dysfunction, and counseling—the latter of which seems to augment the standard treatments).

Figure 3: Professor A.L. Burnett, Baltimore (USA) at #EAU2014
Prof. M. Albersen of Leuven (BE) continued this theme with a review of bench research in erectile dysfunction and the progress of stem cell research. Early work shows potential benefits at the smooth muscle, fibrosis, and innervation endpoints. At least 6 trials are now registered at clinicaltrials.gov in this area, but many are still looking at the safety aspects first. Prof M.J.H. Van Griethuysen ofRotterdam (NL) concluded the session with a review of future research funding.
Congratulations to the organizers and speakers for a strong start to #EAU2014. Where you in the audience? What were your take home messages?
John W. Davis, MD, FACS
Houston, Texas
Associate Editor, Urologic Ongology, BJU International