15th Asia-Pacific Prostate Cancer Conference 2014
Blog author Dr Sarah Wilkinson enjoys lunchtime entertainment at APCC in Melbourne.
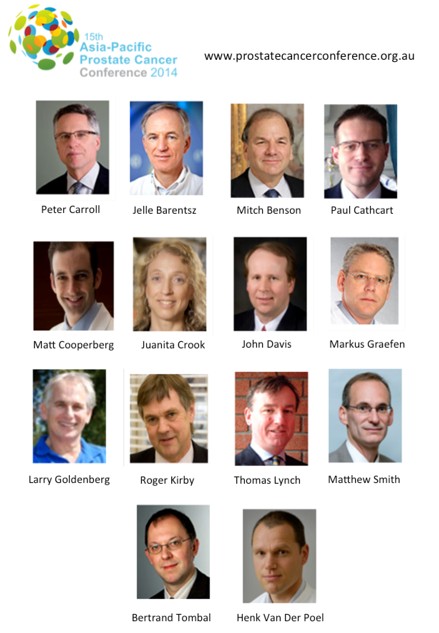
The 15th Asia-Pacific Prostate Cancer Conference 2014 (#apcc14; prostatecancerconference.org.au/) is the largest prostate cancer educational event in the region and attracts over 800 multidisciplinary delegates every year. The world’s leading experts in prostate cancer have featured on the Faculty at this conference in recent year’s and this year’s Faculty was again a great team-sheet for leaders in this field:
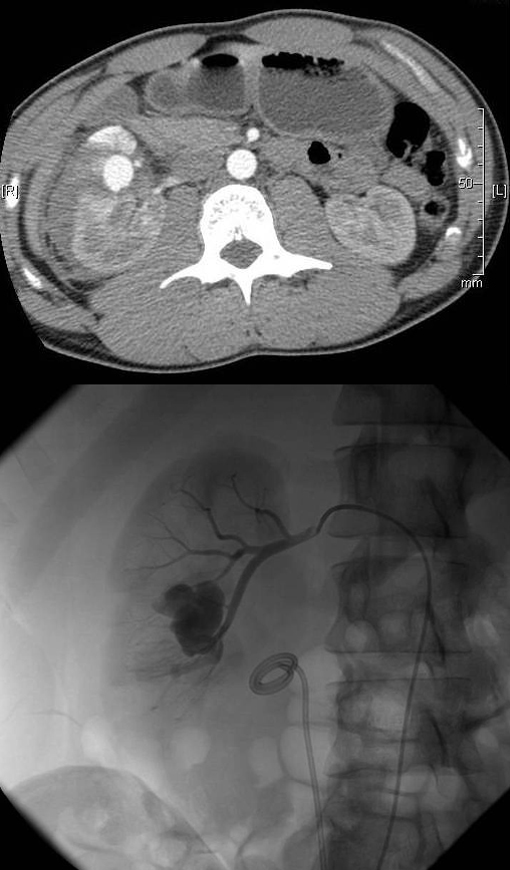
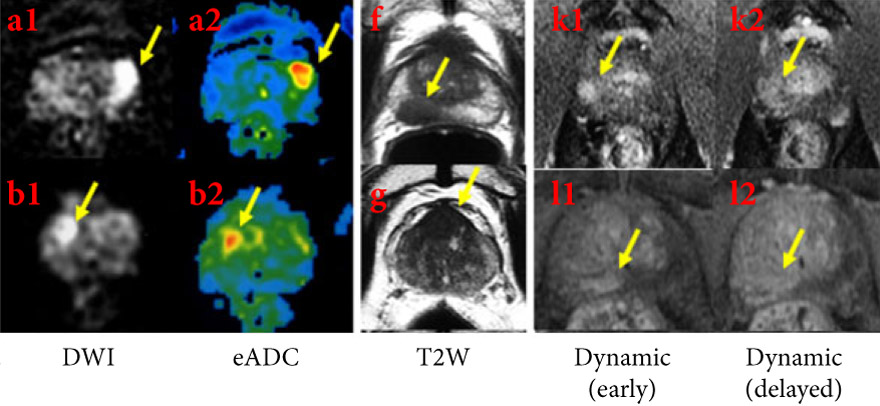
The Confernece kicked off on Sun 31st August with a series of Masterclasses including the very popular da Vinci© Prostatectomy Masterclass (featuring Dr Henk Van Der Poel, Dr John Davis, Dr Markus Graefen and Dr Paul Cathcart), along with new master classes focusing on Prostate MRI scanning (led by Dr Jelle Barentsz), and LDR Brachytherapy (led by Dr Juanita Crook).
MRI Prostate Masterclass led by Jelle Barentsz was a sell-out
The Nursing & Allied Health streams also opened their plenary sessions to a busy auditorium. The official Poster and Welcome Session was held on Sunday evening on what was an unseasonally warm and to Winter in Australia. Whilst enjoying the range of lovely canapés and beverages on offer via Melbourne’s premier conference and catering venue (https://mcec.com.au/), delegates caught up with their long lost urology colleagues and perused the high quality posters on display. Poster prizes were awarded for each of the three conference streams; Clinical Urology, Nursing & Allied Health, and Translational Science, as judged by experts in the respective fields. The task of picking just one winner for the Clinical Urology category proved too difficult for judges A/Prof Henry Woo (@DrHWoo) and Dr Phil Dundee (@phildundee), so a dual prize was awarded to both Dr Fairleigh Reeves (@DrFairleighR) and A/Prof Jeremy Millar (@jeremymillar). Rob McDowell took out the poster prize for the Nursing & Allied Health stream with his poster on baseline characteristics of participants in a telephone-delivered mindfulness intervention for men with advanced prostate cancer. The Translational Science winner was Saeid Alinezhad, who presented; ACSM1, CACNA1D and LMNB1 as three novel prostate cancer biomarker candidates.
Monday morning saw the Official Conference Opening given by conference President Prof Tony Costello (@proftcostello) who announced the opening of a new Royal Men’s Hospital to specifically address the needs of men’s health in Australia. The life expectancy of Australian males is currently 5 yrs less than women, and cancer mortality is a third higher for prostate cancer compared to breast. Rates of alcohol, tobacco and drug abuse, as well as suicide, are all 4x higher in men compared to women. 66% Australian men are overweight or obese, and men are also far less likely to visit their GP for a check-up. Next we were lucky enough to have Federal Minister for Health and Sport, the Hon. Peter Dutton MP (@PeterDutton_MP), take leave from Parliament to give the Ministerial Address. Mr Dutton expressed his support for the conference and the forthcoming opening of the new “Royal Men’s Hospital”, a clinic focussed on Men’s Health in Australia’s premier health science precinct, and spoke of how he hopes the recently proposed $20 billion Medical Research Future Fund will further help advances in this area.
Conference President Prof Tony Costello with Australia’s Minister for Health, Hon Peter Dutton MP
The 2nd Patrick C Walsh Lecture was given by Dr Peter Carroll from the Department of Urology, UCSF, USA. Dr Carroll discussed how we can refine current risk assessments for patients with prostate cancer, and in the process give them refined treatment options. Dr Caroll and his team (including Dr Matthew Cooperberg who was also present), have led the way in risk stratification for men with localised prostate cancer and continue to find ways to best select men at higher risk of adverse outcomes.
This year’s point-counter point debate focused on the preferred method of prostate cancer biopsy. In the left side of the ring we had Mr Jeremy Grummet (@jgrummet) who argued the case for a transperineal biopsy due to multi-drug resistant rectal flora. On the right side we had Mr Shomik Sengupta (@shomik_s) who was in favour of sticking with the well-established TRUS. Following a very close audience vote, session chair A/Prof Nathan Lawrentschuk (@lawrentschuk) declared the winner, “Close, but transfecal by an organism.”
The Conference dinner was held on Monday evening at the Mural Hall, Myer Building. 18th century style mirrored commodes and Parisian inspired parquet flooring transported guests to another world, whilst some fine whisky and entertainment was enjoyed.
And for those who hadn’t partied too hard, the Clinical Urology and Translational Science Breakfast sessions were back by popular demand beginning promptly at 6:45 am the next morning. Both sessions focused on genomics and its implications in diagnosis and treatment planning in what is now coined ‘The Genomic Era’.
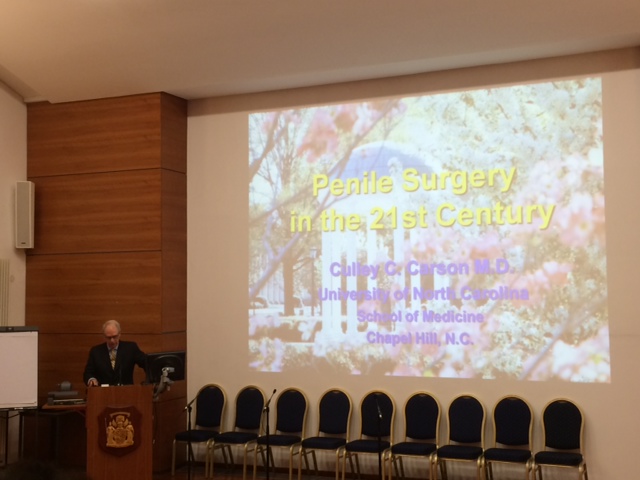
Later in the morning we remembered renowned British urologist Prof John Fitzpatrick, who sadly passed away aged 65 on May 14th 2014, suffering from a massive subarachnoid haemorrhage. His close colleague and friend, Prof Roger Kirby, delivered the remembrance speech “Life in the Fast Lane”, along with a musically accompanied slide show. Prof Kirby’s tribute can also be read here at Blogs@BJUI (https://www.bjuinternational.com/bjui-blog/professor-john-fitzpatrick-1948-2014/).
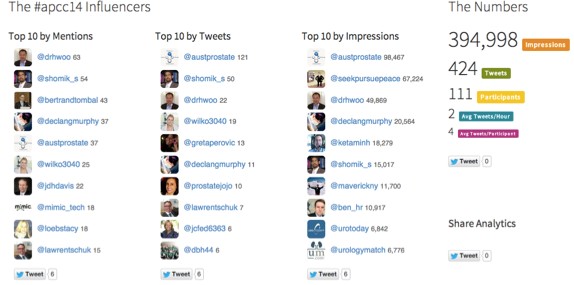
The urology Twitterati were again out in full force at #apcc14. During peri-conference period (including the 5 day lead up period, the actual conference dates, and 2 days post-conference), almost 400,000 impressions were generated in cyperspace from 424 tweets, by 111 participants. There was an average of 2 tweets per hr over the peri-conference period and each participant averaged 4 tweets each.
The conference ended with the exciting news of a 2nd Prostate Cancer World Congress, to be held August 18-21st 2015 in beautiful Cairns, Queensland Australia. See you there!
Sarah Wilkinson completed her PhD in prostate cancer research and is now working as a Medical Science Liaison for Oncology and Haematology at GSK. Twitter: @wilko3040