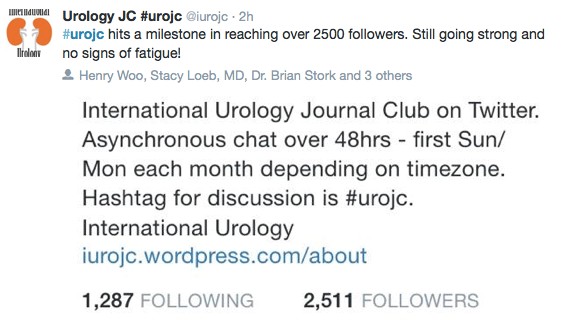
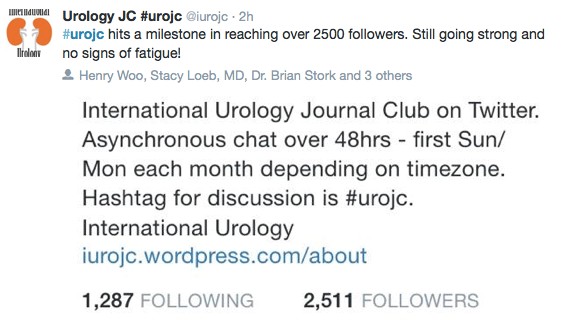
November 2014 ushered in the third year of the international urology journal club (@iurojc) and also marked the 2500th follower of @iurojc.
November 2014 ushered in the third year of the international urology journal club (@iurojc) and also marked the 2500th follower of @iurojc.
 This month’s article was published in European Urology (@Uroweb) on October 10, 2014, Sequential Combination of Mitomycin C Plus Bacillus Calmette-Guerin (BCG) Is More Effective but More Toxic Than BCG Alone in Patients with Non-Muscle-Invasive Bladder Cancer in Intermediate- and High-risk Patients: Final Outcome of CUETO 93009, a Randomized Prospective Trial.
This month’s article was published in European Urology (@Uroweb) on October 10, 2014, Sequential Combination of Mitomycin C Plus Bacillus Calmette-Guerin (BCG) Is More Effective but More Toxic Than BCG Alone in Patients with Non-Muscle-Invasive Bladder Cancer in Intermediate- and High-risk Patients: Final Outcome of CUETO 93009, a Randomized Prospective Trial.
The discussion was once again well attended by many of the Urology twitter gurus and leaders in the field of intravesical chemotherapy for non-muscle-invasive bladder cancer (NMIBC) (@davisbj, @JimCatto, @DrHWoo, @jimmontie, @uretericbud, @shomik_s, @UroDocAsh, etc).
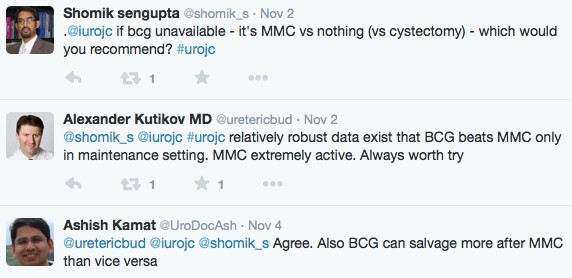
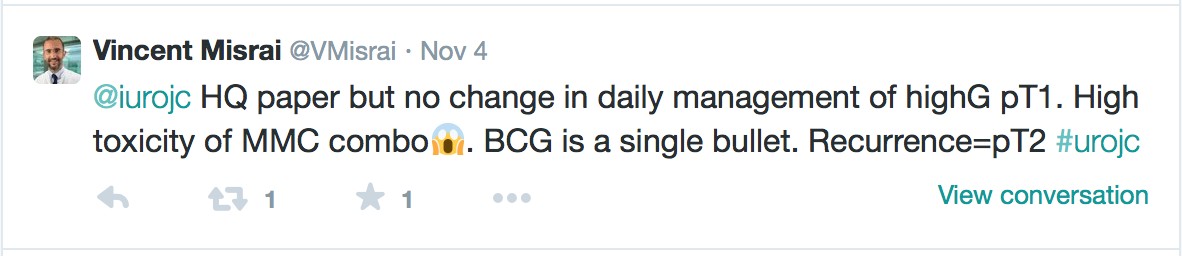
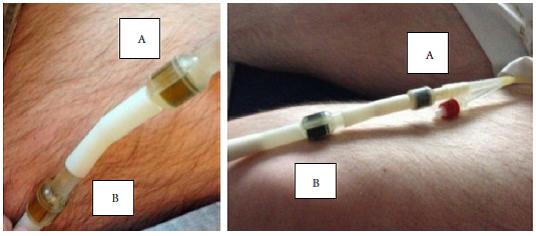
Given the recent worldwide shortage of BCG, this article proved timely for discussion @iurojc. The authors from Spain conducted a prospective, randomized trial including 407 patients with intermediate- to high-risk NMIBC – 211 patients were allocated to receive mitomycin-C (MMC) and BCG, and 196 patients to receive BCG-alone. At 5 years, the disease free interval significantly improved with sequential MMC and BCG compared to BCG alone (HR 0.57, 95%CI 0.39-0.83, p=0.003), and reduced the relapse rate from 33.9% to 20.6%. However, sequential treatment lead to increased toxicity even after lowering the MMC dose to 10mg (p<0.001). The authors concluded that due to higher toxicity, sequential MMC and BCG therapy should only be given to patients with high likelihood of tumor recurrence (ie. recurrent T1 tumors).
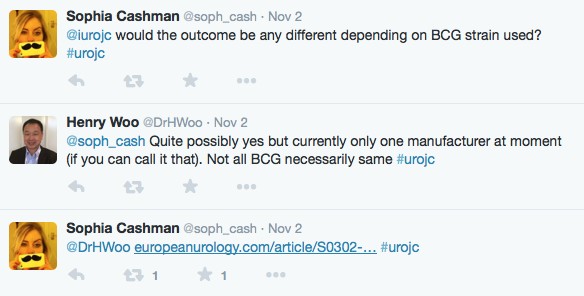
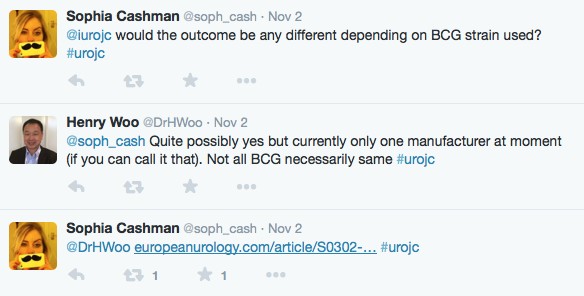
The discussion started with the point being made that BCG strain may influence outcomes, with reference made to the @Uroweb article discussing the outcomes of NMIBC and BCG strain.
Subsequently, we were reminded that patients with recurrent T1 tumors are at high risk for disease progression and mortality, and that appropriately fit patients should be offered aggressive treatment (radical cystectomy).
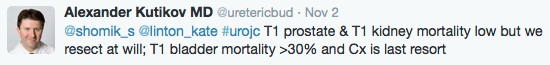
@uretericbud also made the point that we aggressively treat T1 prostate and T1 kidney cancer, which have low cancer specific mortality, however cystectomy is the last resort for T1 bladder cancer (mortality >30%).
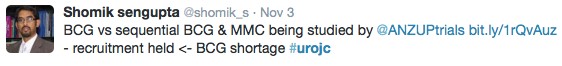
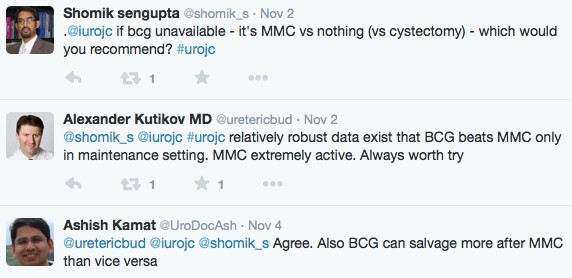
The reality of the worldwide BCG shortage was also highlighted during the discussion, ultimately affecting other ongoing MMC and BCG trials.
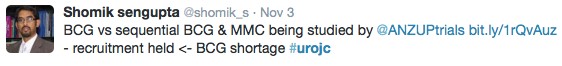
This month’s discussion concluded with a conversation regarding treatment options during the BCG shortage. The conclusion among the discussants was for MMC during the induction phase of treatment.
Overall, the consensus was that although the results of MMC and BCG in sequence are encouraging, appropriately fit patients may still benefit from radical cystectomy for recurrent T1 disease. With the worldwide shortage of BCG, perhaps this decision will be easier to make. Happy #movember everyone.
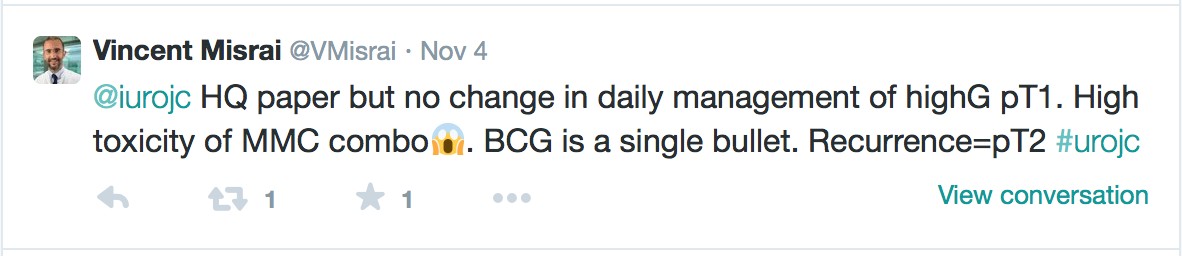
The winner of the Best Tweet prize is Vincent Misrai who will receive a complimentary registration to the USANZ Annual Scientific Meeting to be held in Adelaide, Australia in March 2015.
Thank you to the Urological Society of Australia and New Zealand (USANZ) for providing this generous prize. Thanks also to European Urology for enabling this paper to be open access for the November #urojc.
Zach Klaassen is a Resident in the Department of Surgery, Section of Urology Georgia Regents University – Medical College of Georgia Augusta, USA. @zklaassen_md