Final Analysis of RT+ADT versus ADT alone in locally advanced CaP
 The March 2015 international urology journal club #urojc twitter discussion focused on a paper by Mason et al [1]. This article, published in the Journal of Clinical Oncology (Feb 2015), reports on the preplanned final analysis of the randomized trial of radiotherapy (RT) and androgen deprivation therapy (ADT) versus ADT alone in patients with locally advanced prostate cancer between 1995 and 2005.
The March 2015 international urology journal club #urojc twitter discussion focused on a paper by Mason et al [1]. This article, published in the Journal of Clinical Oncology (Feb 2015), reports on the preplanned final analysis of the randomized trial of radiotherapy (RT) and androgen deprivation therapy (ADT) versus ADT alone in patients with locally advanced prostate cancer between 1995 and 2005.
The authors have previously reported on the survival benefits of RT added to ADT in this cohort of patients and the final analysis demonstrates a sustained longer-term survival outcomes of RT+ADT over a median follow-up of 8 years as compared to ADT alone.
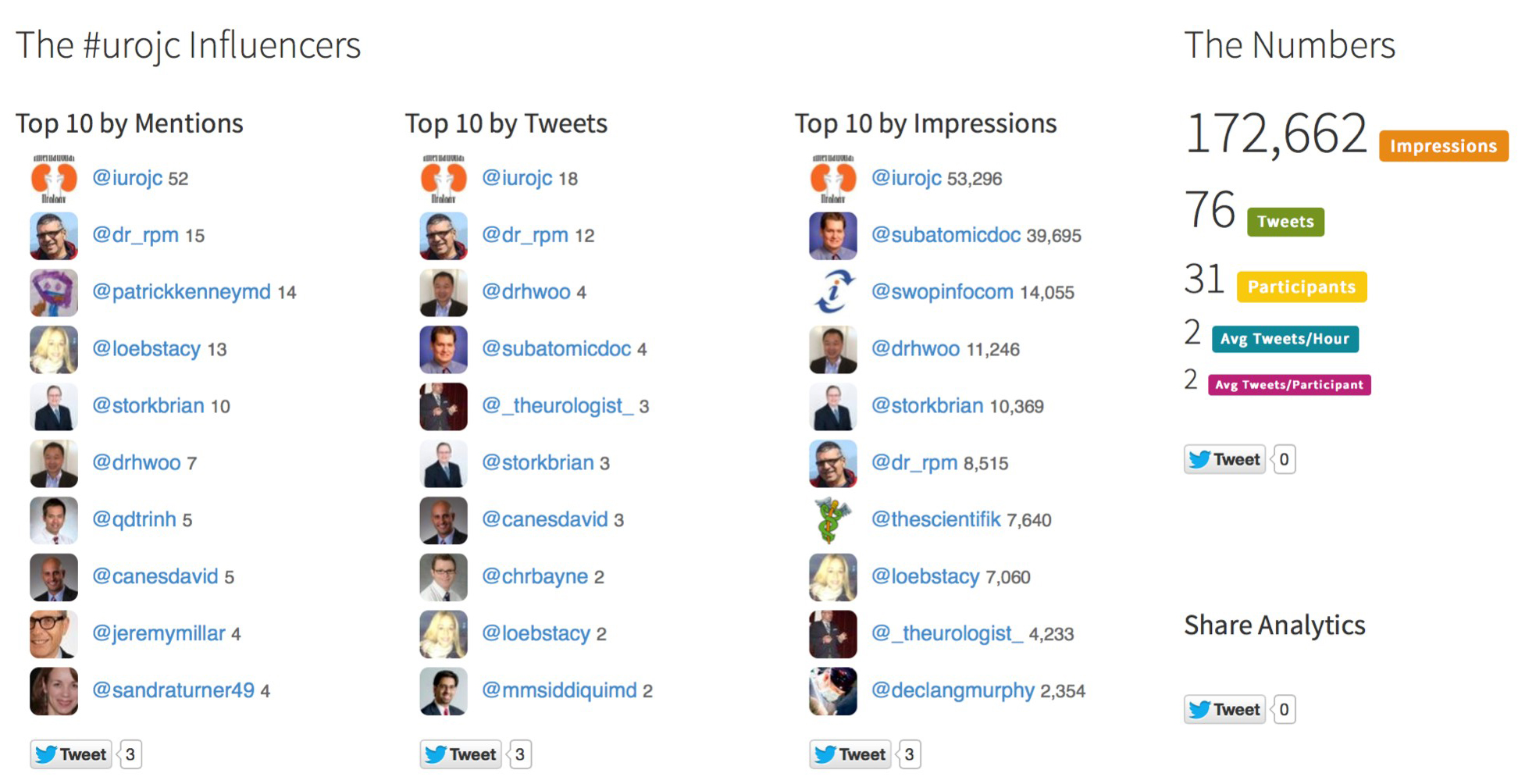
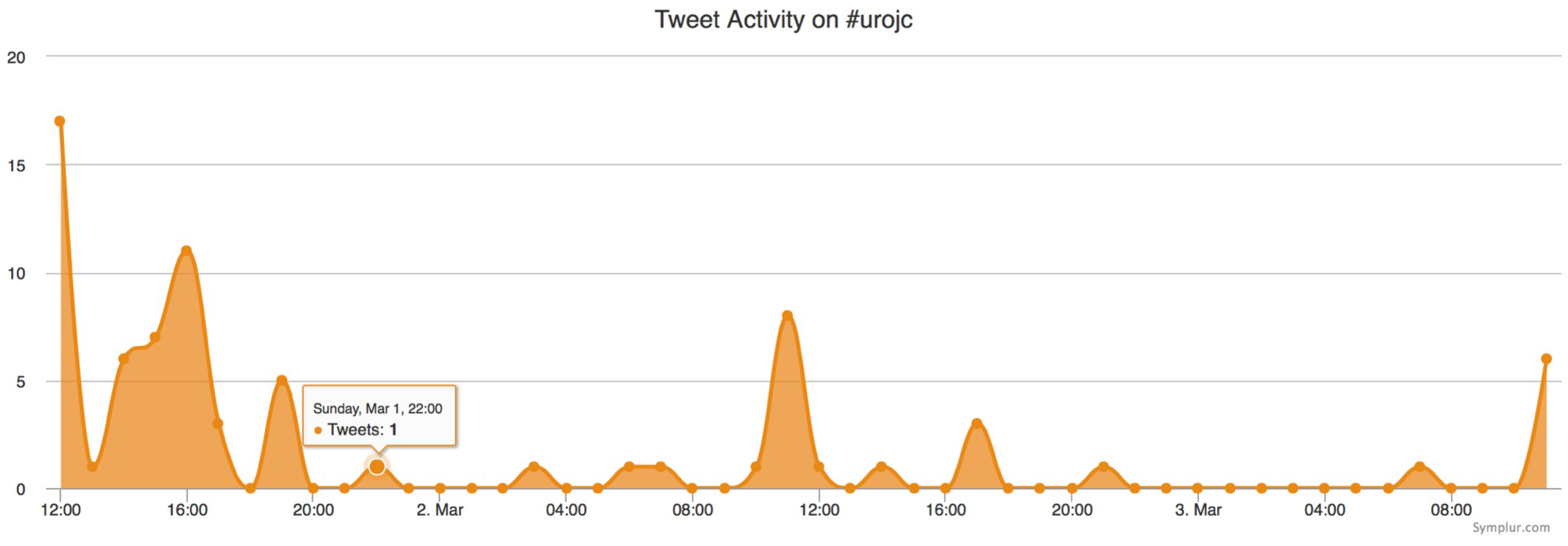
As ever the discussion was lively with some polarized views. The feed commenced at 12:00pm PST on Sunday 1st March 2015 for a 48-hour period. Initially debate focused on staging and the under-reporting of DRE findings:
Which was perhaps addressed by issues during the screening process…
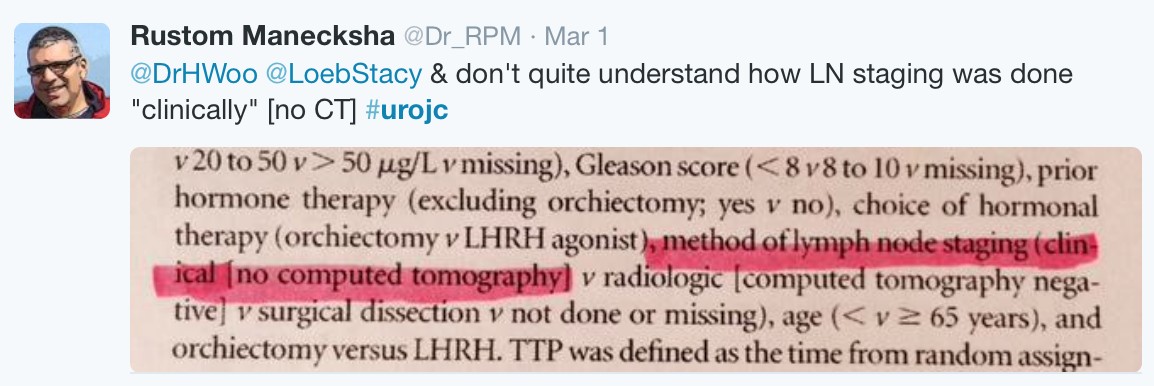
Despite this, other aspects of staging were discussed, particularly the methods for node staging:
For N staging, the authors included either a clinical assessment (70.5% of patients), Imaging (8.5%) or surgical dissection (2.4%). Meanwhile, the accuracy of ‘clinical’ nodal staging was questioned.
Consideration of the patient inclusion criteria was followed by a discussion over the use of ADT in this patient cohort
In this context, ADT consisted of either BSO or lifelong LHRH agonists
However, the question was asked of ADT in addition to RT ‘is lifelong ADT appropriate?’
While for high-risk disease, evidence suggests that long-term (2-3 years) ADT should be used following RT [2, 3], for intermediate risk cancers, 8 weeks of adjuvant ADT remains the standard of care as highlighted in the recent RTOG 9910 data [4].
The rationale behind RT and ADT was noted:
While the results of the study came as no shock to some:
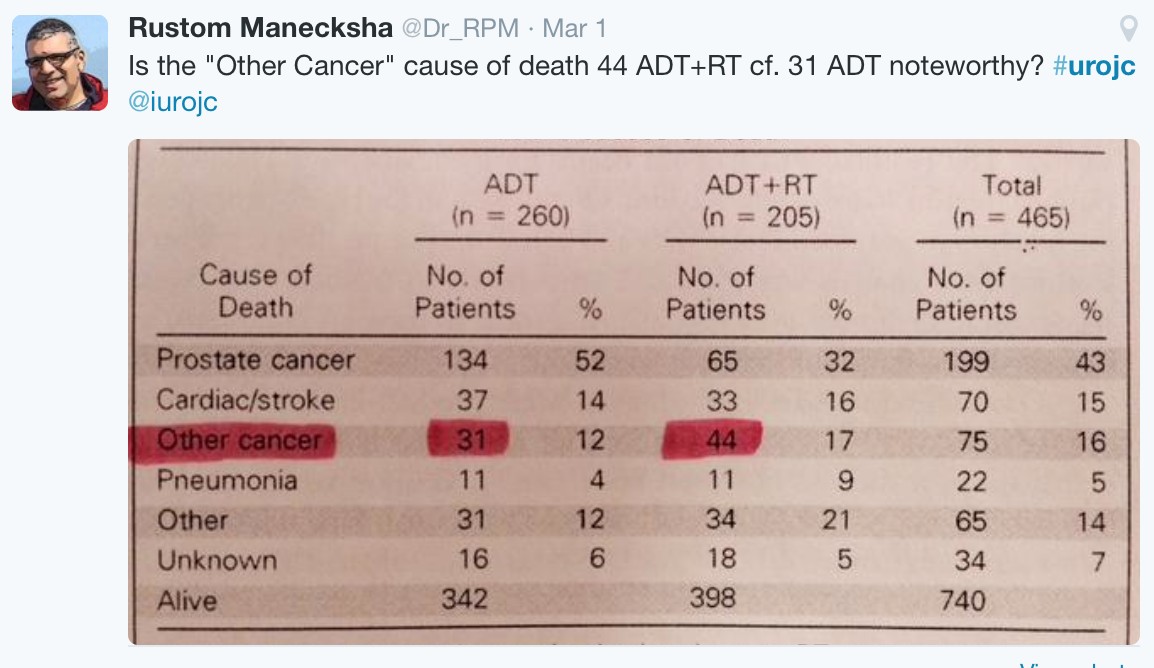
The addition of RT to ADT significantly improved OS and DSS. The study reports that ‘there was no evidence of any differences in deaths from other causes’, however, the issue of secondary malignancies with RT was ‘highlighted’:
Ultimately, the role of surgery for these patients was questioned. A point highlighted in the paper was not shared by some:
To conclude the March #urojc, some final comments were provided by @_TheUrologist:
Thanks to all those who participated in this months discussion. We look forward to the April #urojc.
[1] Mason, M.D., W.R. Parulekar, M.R. Sydes, et al., Final Report of the Intergroup Randomized Study of Combined Androgen-Deprivation Therapy Plus Radiotherapy Versus Androgen-Deprivation Therapy Alone in Locally Advanced Prostate Cancer. J Clin Oncol 2015;.
[2] Horwitz, E.M., K. Bae, G.E. Hanks, et al., Ten-year follow-up of radiation therapy oncology group protocol 92-02: a phase III trial of the duration of elective androgen deprivation in locally advanced prostate cancer. J Clin Oncol 2008;26:2497-504.
[3] Bolla, M., G. Van Tienhoven, P. Warde, et al., External irradiation with or without long-term androgen suppression for prostate cancer with high metastatic risk: 10-year results of an EORTC randomised study. Lancet Oncol 2010;11:1066-73.
[4] Pisansky, T.M., D. Hunt, L.G. Gomella, et al., Duration of androgen suppression before radiotherapy for localized prostate cancer: radiation therapy oncology group randomized clinical trial 9910. J Clin Oncol 2015;33:332-9.
Chris Hillary @chrisjhillary
Clinical Fellow in Urology, Sheffield, UK