When Not to be a Doctor
“Now you know. And knowing is half the battle.” As a child growing up in the 80’s, I heard this line at the end of every G.I. Joe cartoon show. But what if knowing doesn’t really help?
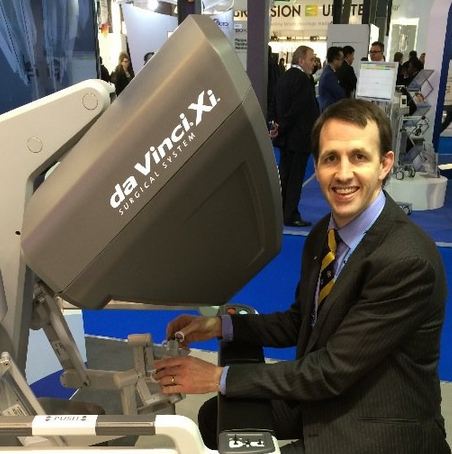
As a urologic oncologist, I (try) to know as much as possible about urology and urologic cancers. I counsel patients about their diagnosis, treatment, and prognosis. I give them facts and statistics, quote predictive nomograms, describe operations, draw pictures, and give them my expert opinion. I would like to think that I am being helpful.
But am I really helping? Do patients and family members really want all of that?
Twenty years ago, my mother-in-law had breast cancer. She had a lumpectomy, chemotherapy and radiation. She “cured” and went on with her life. Her cancer was mentioned occasionally, but only as a remote event. We mostly forgot about it.
Then, 4 years ago, she felt a lump next to her breast. Eventually it was biopsied – recurrent breast cancer. She saw the experts at my hospital. Bad news – the cancer had spread (in a big way) to her liver.
We were all devastated, especially my wife. After 10 years away, she had just moved back to New England. She was looking forward to spending more time with her mom and her family. Cancer had reared its ugly head, and turned that all upside down.
What did I do? I did what I thought would be helpful. Looked up treatment options. Looked up 5-year survival estimates. I gathered information. Lots of information. This turned out to be an unmitigated disaster. It did not help my wife. It made things worse.
In 2014, Paul Kalanithi, then a Neurosurgery resident at Stanford, wrote a great piece in the New York Times about his advanced lung cancer diagnosis.
His basic message – don’t obsess over the numbers. Live your life. Get on.
I had failed my wife in that moment by acting like “a doctor”. She didn’t want numbers or survival estimates. She wanted me to act like a husband and friend. She wanted sympathy, a hug, and a shoulder to cry on. She wanted me to acknowledge how much it sucked that her mom had cancer.
In the end, patients want both, and they need both. They need expert advice and “the numbers”. More importantly, they want and need compassion and empathy. Thankfully, my mother-in-law continues to do well to this day.
Communicating both of these effectively will make me a better doctor, a better husband, and a better person.
Dr Matt Hayn
Medical Direction, Genitourinary Cancer Program
Maine Medical Center
Portland, Maine
@matthayn