Video: Multiple Growth Periods of SRMs Predict Unfavourable Pathology
Multiple growth periods predict unfavourable pathology in patients with small renal masses
Abstract
Objective
To use the number of positive growth periods as a characterization of the growth of small renal masses in order to determine potential predictors of malignancy.
Patients and Methods
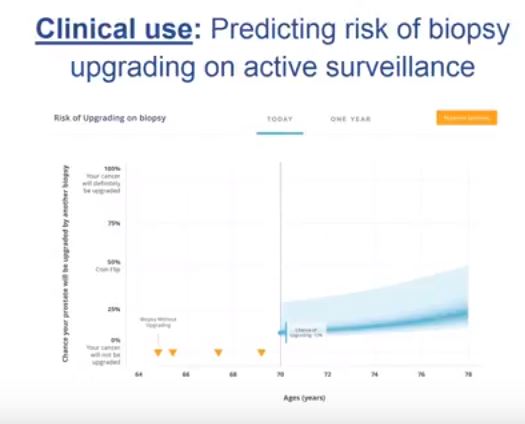
Patients who underwent axial imaging at multiple time points prior to surgical resection for a small renal mass were queried. Patients were categorized based on their pathological tumour grade and stage: favourable (benign, chromophobe and low‐grade pT1–2 renal cell carcinoma [RCC]) vs unfavourable (high‐grade of any stage and low‐grade pT3–4 RCC). A positive growth period was counted each time the difference in greatest tumour diameters between two images was positive. The Cochran–Armitage trend test and Somers’ D association were used to determine if the number of positive growth periods was correlated with unfavourable pathology.
Results
Of the 124 patients, 86 (69.4%) had favourable pathology and 38 (30.6%) had unfavourable pathology. Those who had favourable pathology were younger than those who had unfavourable pathology: median (interquartile range [IQR]) 61.0 (52.2–66.0) vs 68.5 (61.5–77.0); P < 0.001. The overall growth rate was higher in the unfavourable group, but was not statistically significant: mean (sd) 0.7 (1.7) vs 1.6 (2.8) cm/year; P = 0.07. There was a significant trend difference in the number of positive growth periods between favourability groups (P = 0.02). An association between increased number of positive growth periods and unfavourable pathology was observed: 0.15 (95% confidence interval 0.02, 0.29). The ratios of favourable to unfavourable pathology were 1.8, 1.0, 0.66, 0.59 and 0 as the number of positive growth periods increased from 0 to 4, respectively.
Conclusion
While overall growth rate was not predictive of pathology favourability, there was a positive association between the number of positive growth periods and unfavourable pathology. The number of positive growth periods may be a potential parameter for malignant potential in patients undergoing active surveillance for small renal masses.