Editorial: Do you need further assistance in diagnosing and risk stratifying prostate cancer?
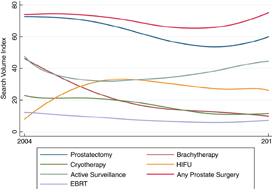
I would hope the answer to the question posed in the title is a universal ‘yes’; at least that is my experience with this complex and common disease. The concept that in 2019, we have unmet needs in prostate cancer diagnostics is somewhat remarkable, given that we have access to: (i) one of the most widely used biomarkers in oncology (PSA), (ii) a readily accessible organ to examine (DRE), (iii) state of the art imaging (MRI, positron emission tomography), (iv) specialty biopsy systems (fusion/transperineal template), (v) enhanced risk stratification systems (National Comprehensive Cancer Network [NCCN], Cancer of the Prostate Risk Assessment [CAPRA], etc.), (vi) numerous nomograms, (vii) secondary urine/serum biomarkers (Prostate Health Index [PHI], prostate cancer antigen 3 [PCA3], SelectMDx, ExoDx, four‐kallikrein panel [4K]), and (viii) commercially available genomic platforms (Prolaris, OncotypeDx, Decipher).
The paper by Connell et al. [1] in this issue of BJUI asks you to consider adding another diagnostic test to your list. You might correctly assume from the title that the test is in discovery/validation stages, and lacks a fancy commercialised name. Many steps await any promising biomarker to make it to your clinic. So why pay attention to this one? Let me reiterate a few points made by the authors and suggest where new paradigms might emerge if the test delivers on its promises.
First, the test crosses over the current barriers between screening patients and active surveillance (AS). In both populations we care about Gleason Grade Group ≥2. Yet a SelectMDx or similar tests are validated for diagnosis but not for monitoring Grade Group 1 on AS. Genomic profiling tests have strong validation and prognostic value for AS, but require tissue and external laboratory work flows. This marker is being tested for both settings, with potentially meaningful distinctions for both patient groups.
Second, this test is in the urine and does not need imaging or needles to obtain samples. It may have serial use (if cost‐effective) for monitoring AS.
Third, for AS cohorts, the test seems to be able to identify progression well in advance. This would potentially allow for early intervention in the correct patients, and less intense monitoring in the remaining.
Fourth, the test metrics looked favourable in PSA screened and unscreened populations; will we ever see a novel biomarker bold enough to move to primary/independent screening status?
Fifth, some of the secondary biomarkers you may be using now are included in this model: PCA3, transmembrane protease serine 2:v‑ets erythroblastosis virus E26 oncogene homolog (TMPRSS2‐ERG), Homeobox C6 (HOXC6).
To be critical, this biomarker will need significant validation in other cohorts, and we can always hope for head‐to‐head data with existing strategies. I will remain optimistic these authors can move this biomarker strategy along and help bridge some of the gaps that remain in disease detection and risk stratification. I may even attempt to insert some of those lovely new equations in the methods section into future lectures.
Reference
- , , et al. A four‐group urine risk classifier for predicting outcomes in patients with prostate cancer. BJU Int 2019; 124: 609– 20