Editorial: Vaporization is vaporization, but not at any cost…
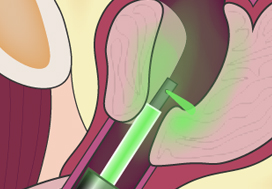
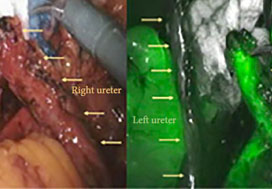
The paper by Ghobrial et al. [1] confirms that bipolar electrocautery vaporization is more cost‐effective than GreenLight Laser vaporization, as the two techniques are equally effective but GreenLight vaporization is more costly in the smaller prostates being studied.
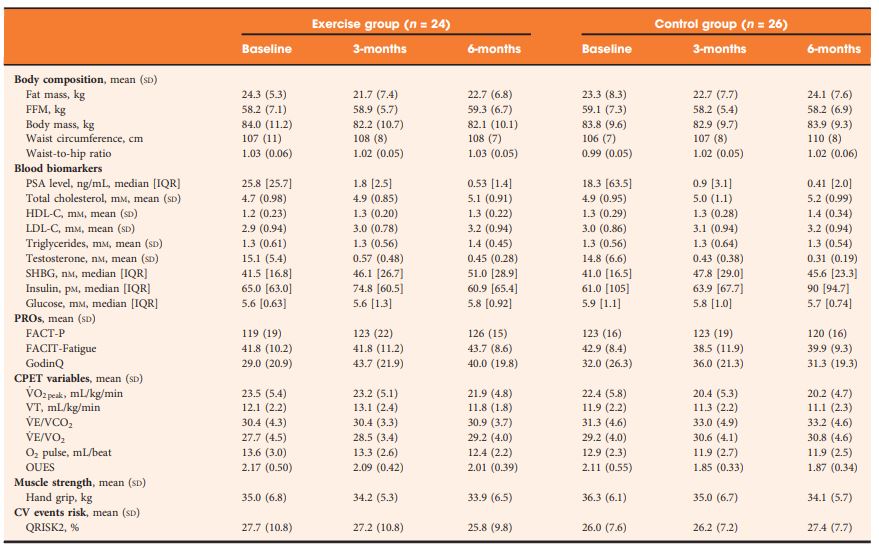
Underpinning the analysis was a well‐conducted randomized controlled trial, showing equivalent peri‐operative and postoperative measures with the two procedures and no difference in the primary endpoint of IPSS reduction at 2 years. The two techniques were performed in a similar manner and were equally efficient and safe as expected.
Philosophically, the clinical results are both unsurprising and expected, and confirm the long‐held belief that the energy source employed for vaporization and, for that matter, enucleation, is of secondary concern compared to the skill and dedication of the operator. The technique in either case should result in comparable efficacy, leaving cost‐effectiveness to be an important way to help both urologists and administrators discriminate between them.
Although the costs are not necessarily going to be comparable with those in other jurisdictions, this will apply equally to both treatments and this study therefore represents an excellent attempt to cost both procedures, removing equivalent costs. Importantly, this assessment included the costs of both readmissions and interventions over the full 24‐month period. This captures the bulk of the important complications after these types of procedures and adds to the validity of the findings.
The big difference between the costs of the two treatments being studied is, of course, ‘capital equipment including maintenance’. The single‐use fibre model rather than the cost of the machine has been the mainstay for the profitability of laser companies since the inception of laser prostatectomy. The maintenance contract has been a further cost, which is always underestimated. Reusability of the laser fibres is one way of diminishing per‐procedure costs, but is only consistently possible for Holmium end‐fire fibres [2]. The fact that the authors estimate of these costs was a ‘case share in 5‐year budget plan’ also suggests that the true cost of the use of the GreenLight laser is underestimated.
With the burgeoning number of new techniques and technologies for the treatment of BPH emerging, and new treatment paradigms being proposed, let alone the increasingly negative focus on medical waste [3] and the increasing use of single‐use disposable handpieces/tubing/drapes/fibres, articles such as this are timely. A standardized methodology for assessing the cost‐effectiveness of treatments for BPH is needed and should be an essential part of pivotal studies and therefore the regulatory approval processes.
by Peter Gilling
References
- , , et al. A randomized trial comparing bipolar transurethral vaporization of the prostate with GreenLight laser (xps‐180watt) photoselective vaporization of the prostate for treatment of small to moderate benign prostatic obstruction: outcomes after 2 years. BJU Int. 2020; 124: 144– 52
- , , , . Holmium laser resection of the prostate is more cost effective than transurethral resection of the prostate: results of a randomized prospective study. Urology 2001; 57: 454– 8
- , , , , , . Evaluation of operative waste in a military medical center: analysis of operating room cost and waste during surgical cases. Am Surg. 2019; 85: 717– 20