Editorial: Nationwide prostatectomy practice
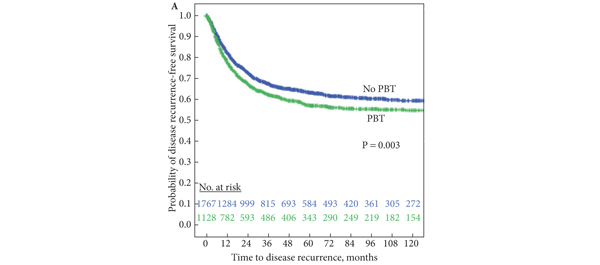
Surgical management of prostate cancer is one of the most frequently performed urological procedures [1]. Available data suggests that surgeons’ experience is correlated with both oncological and functional outcome [2]. These initial observations stress the importance of concentration of prostatectomy in high-volume institutes. This centralisation could improve documentation and monitoring of outcome. The data presented by Røder et al. [1] from Denmark show a rapid increase in registered prostatectomy procedures in recent years in six institutes. It remains to be studied whether this is caused by centralisation and better registration or the results of an increased overtreatment. For that, data on the incidence of low-risk disease over time in their series needs analysis.
At least one-third of the population was treated since 2008. The relatively short follow-up and associated few events, and high number of low-risk patients (47% had biopsy Gleason ≤6) make outcome analysis of less value. It is therefore not surprising that in their analysis low- and intermediate-risk tumors had similar outcome. On the other hand, despite prostatectomy, one-third of deaths during follow-up were prostate cancer related in their population. Consistent with reported data at 15 years after prostatectomy more patients died from prostate cancer than from other causes [3]. But still a considerable number of men died from prostate cancer. This also seems the case in the group of men often soothed for having indolent, low-risk disease. At 15 years Røder et al., reported 8.9% of these men with low-risk disease still dying from prostate cancer in Denmark, despite prostatectomy. And although this percentage was lower than that of the prostatectomy group in the Scandinavian Prostate Cancer Group Study Number 4 (SCPG-4) study (14.6%) [4], most men will still find it disturbingly high and it is three-times higher than the 3% life-time risk of dying from prostate cancer for all men. In other words, it may be perceived that prostatectomy does only partly reverse the risk of dying from prostate cancer, even in men with low-risk disease.
The data from Røder et al. [1] can, with longer follow-up, set the standard for oncological outcome on a national level. Of interest is the observation that, although not significant in the multivariate analysis, variation among institutes for outcome seems to exist but not clearly dependent on institutes volume. Variations of case-mix and patient selection could be topics of further study. With the short follow-up available we are also looking forward to data on functional outcome and perioperative complications that may be more mature. Comparison with now also available registries in Belgium and the Netherlands would be of interest.
It always strikes me that prostate cancer seems to be a systemic disease from the start even in assumed ‘low-risk’ disease, yet surgical management is only focused at loco-regional control. Perhaps the mortality improvement shown in the Scandinavian Prostate Cancer Group Study Number 4 (SPCG-4) trial by prostatectomy is merely caused by disease delay provided by local control even in the presence of systemic disease. Initial encouraging data from an ongoing study evaluating the role of radiotherapy to the prostate in the presence of bone metastases seem supportive of this notion. Is prostatectomy a debulking management of a systemic disease at most, and an unneeded cure for many, or is there this sub-sub group of men that is eventually fully benefiting from the intervention reversing not only death but also the debilitating effects of androgen ablation.
References
- Røder MA, Brasso K, Christensen IB et al. Survival after radical prostatectomy for clinically localised prostate cancer: a population-based study. BJU Int 2014; 113: 541–547
- Vickers A, Savage C, Bianco F et al. Cancer control and functional outcomes after radical prostatectomy as markers of surgical quality: analysis of heterogeneity between surgeons at a single cancer center. Eur Urol 2011; 59: 317–322
- Shikanov S, Kocherginsky M, Shalhav AL, Eggener SE. Cause-specific mortality following radical prostatectomy. Prostate Cancer Prostatic Dis 2012; 15: 106–110
- Bill-Axelson A, Holmberg L, Ruutu M et al. Radical prostatectomy versus watchful waiting in early prostate cancer. N Engl J Med 2011; 364: 1708–1717