A test to exclude the presence of aggressive prostate cancer would be highly desirable. In the article by Wysock et al. [1], the authors examine pathological results in 75 men who underwent 12-core systematic biopsy using the Artemis device; all had a pre-biopsy MRI showing no suggestion of cancer. In 74 patients no cancer with Gleason score ≥7 was found on biopsy, which translates into a remarkable 98.7% negative predictive value (NPV) for potentially aggressive disease. The implication is that virtually all serious prostate cancers can be seen on MRI, and thus a negative MRI obviates the need for a biopsy. If this finding were to be confirmed, the majority of prostate biopsies could be avoided, a truly laudable goal.
However, for several reasons, we are not yet able to endorse the blanket concept, ‘get a negative MRI and skip the biopsy’. The authors acknowledged their study is not definitive: it is a retrospective look at 29% of eligible participants; how were they chosen? Further, the ‘gold standard’ for identifying cancer, microscopic examination of whole mount prostatectomy specimens, was not available. Thus, the data presented are striking because of the near-perfect findings, but not entirely convincing. Our work, involving >2 000 MRI/ultrasound-fusion biopsies, teaches that if biopsy is indicated on clinical grounds e.g., palpable abnormality, family or racial history, persistent PSA suspicion, a negative MRI should not preclude a systematic (template) biopsy [2]. Clinical information, especially increased PSA density, may help to select patients for biopsy beyond use of MRI data alone.
Another reason why a ‘negative’ MRI should not always negate the need for biopsy relates to the current proliferation of prostate MRI studies. Many of the new MRI studies are being performed and interpreted by radiologists not adequately trained in this niche. Despite attempts at standardisation [3], the variability of MRI readings, from place to place and from one radiologist to another, can be remarkable. In the recent past I have seen lesions called Prostate Imaging-Reporting and Data System (PI-RADS) Grade 5 ‘disappear’ when scrutinised by more-experienced readers; the reverse has also been seen. Even among expert readers using the latest Version 2 of PI-RADS, agreement in prostate MRI interpretation is only moderate at best (κ ≈0.5) [4]. Therefore, widely varying interpretations of prostate MRI can be expected for the near-term future. A formal training programme and certification in MRI interpretation, which is sorely needed, has not yet been established.
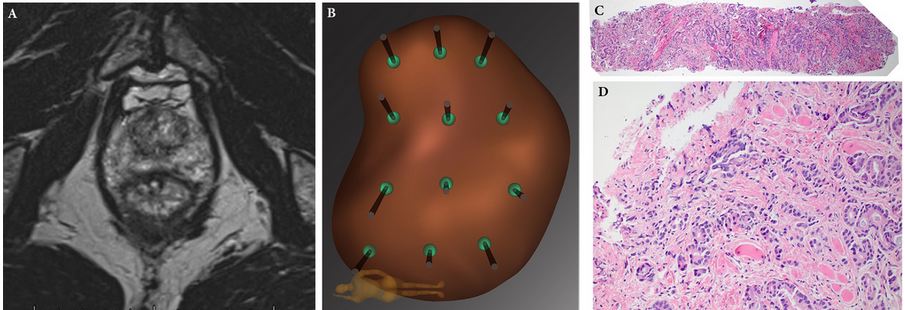
In Figure 1 above, a falsely negative MRI from our institution is shown [2]. The MRI-invisible cancer is not a rarity. In a consecutive series of 1 042 men undergoing template biopsy regardless of MRI findings, the incidence of clinically significant prostate cancer in men with no MRI-suspicious lesions (biopsy-naïve subgroup) was 12% [5]. Further, when looking carefully at whole-mount prostatectomy specimens, the incidence of clinically significant prostate cancer not seen on expertly read MRI was 28% [6]. Still further, some Gleason 6 cancers thought to be insignificant may have the biological potential for de-differentiation [7] and require follow-up. Therefore, at this point in time, a negative MRI should not preclude prostate biopsy, which otherwise would be indicated on clinical grounds. We are still learning about prostate MRI!
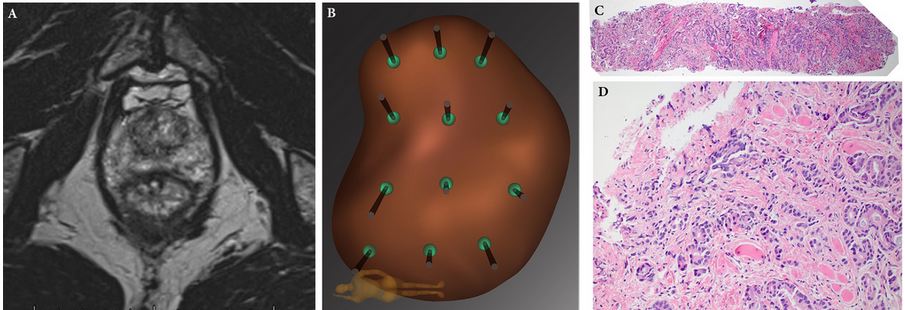
Figure 1: Example of falsely negative MRI. Patient was a Caucasian male (PSA level 3.8 ng/mL) aged 68 years, who on a previous conventional biopsy was found to have a microfocus of Gleason 3 + 3 = 6 prostate cancer. He was considered for active surveillance, and multiparametric MRI of prostate was obtained (A): prostate volume was found to be 35 mL; no region of interest was identified. Mapping biopsy was performed by following the 12-point template of the Artemis device (B). A tissue core from the left lateral apex revealed 6 mm of Gleason 3 + 5 = 8 prostate cancer (C, ×4; D, ×20). Radical prostatectomy was performed, revealing a tumour on the left side of the prostate with diameters of 15 × 12 × 9 mm. Falsely negative MRI is not uncommon. When biopsy is clinically indicated, a negative MRI should not preclude mapping biopsy. Reproduced with permission from Nassiri et al., 2015 [1].
Leonard S. Marks
Professor and deKernion Endowed Chair, Department of Urology, David Geffen School of Medicine at UCLA, Los Angeles, CA, USA
1 Wysock JS, Mendhiratta N, Zattoni F et al. Predictive value of negative 3T multiparametric magnetic resonance imaging of the prostate on 12-core biopsy results. BJU Int 2016; 118: 515–20
2 Nassiri N, Natarajan S, Margolis DJ, Marks LS. Targeted prostate biopsy: lessons learned midst the evolution of a disruptive technology. Urology 2015; 86: 432–8
3 Weinreb JC, Barentsz JO, Choyke PL et al. PI-RADS Prostate Imaging – Reporting and Data System: 2015, Version 2. Eur Urol 2016; 69: 16–40
4 Rosenkrantz AB, Ginocchio LA, Cornfeld D et al. Inter-observer reproducibility of the PI-RADS Version 2 Lexicon: A multi-center study of six experienced prostate radiologists. Radiology 2016; 280: 793–804
5 Filson CP, Natarajan S, Margolis DJ et al.Prostate cancer detection with magnetic resonance-ultrasound fusion biopsy: The role of systematic and targeted biopsies. Cancer 2016; [Epub ahead of print]. doi: 10.1002/cncr.29874
6 Le JD, Tan N, Shkolyar E et al. Multifocality and prostate cancer detection by multiparametric magnetic resonance imaging: correlation with whole-mount histopathology. Eur Urol 2015; 67: 569–76
7 Palapattu GS, Cani AK, Huang J et al. Progression of low- to high-grade prostate cancer: Molecular profiling of tissue obtained by serial targeted biopsy. J Clin Oncol 2015; 33 (Suppl.): Abstract 501