Editorial: sLND – if yes, Robotics?
The manuscript in this issue of the BJUI by de Castro Abreu et al. [1] reports the results of the first series of patients to undergo robotic-assisted salvage lymph node dissection (sLND) for nodal recurrence of prostate cancer. Despite the absence of a high level of evidence, sLND has been gaining attention in recent years. Indeed, several series have shown promising results of such an approach, especially in terms of PSA response to surgery and delay in clinical recurrence [2-4]. However, sLND is a complex surgery and is not devoid of complications, as in up to 13.8% of patients Clavien–Dindo ≥IIIa complications occur [5]. When analysing the results of the current manuscript [1], it is impressive to read that the mean number of LNs removed was 83, ranging from 41 to 132, which is significantly higher than the reported figures of open sLND series. Moreover, despite the long median operative time (4.8 h), complication rates and postoperative course were excellent as compared to previously published series, although a direct comparison between the open and robot-assisted approach should be only addressed in prospective studies. The authors should be congratulated on the superb results obtained during the learning curve of such complex surgery, but some issues need to be discussed.
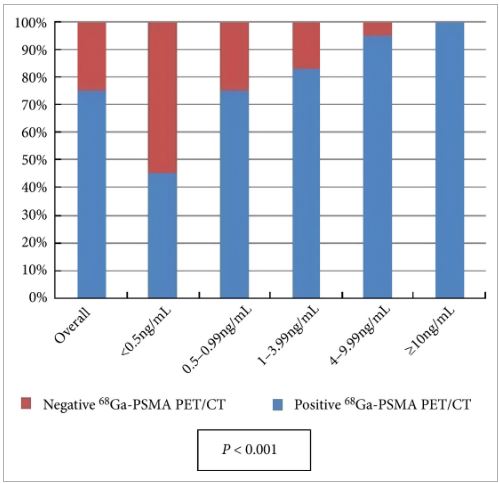
First, it is difficult to understand whether such results apply only to very expert surgeons. In other words, is it possible to translate such surgery to less experienced robotic surgeons? Second, is it necessary to extend the LND to a similar extent in all cases? Previous reports have shown that patients with retroperitoneal involvement may not benefit from sLND as much as their counterparts with only pelvic involvement [2]. The authors [1] show no significant impact of such an extended approach on complications and postoperative course, but the invasiveness of such an extended approach needs to be justified in each case. Third, the introduction of new tracer methods, such as prostate-specific membrane antigen (PSMA) positron emission tomography/CT, with higher specificity for prostate cancer may reduce the need for such extended templates, without compromising the oncological results [6]. Fourth, is the robotic approach feasible and safe in patients previously submitted to radical prostatectomy independently from the approach (open vs laparoscopic/robotic), from the extent of the previous LND, as well as from the previous administration of adjuvant/salvage radiotherapy? All these answers will need to be addressed in future studies on subgroups of patients undergoing sLND. Most importantly, until a high level of evidence is available, sLND should still be considered experimental and should be performed by highly experienced surgeons.