Video: Surgical outcomes of PCNL and results of stone analysis
Surgical outcomes of percutaneous nephrolithotomy in 3402 patients and results of stone analysis in 1559 patients
Abstract
Objective
To report our experience of a series of percutaneous nephrolithotomy (PCNL) procedures in a single centre over 18 years in terms of patient and stone characteristics, indications, stone clearance and complications, along with the results of chemical analysis of stones in a subgroup.
Patients and Methods
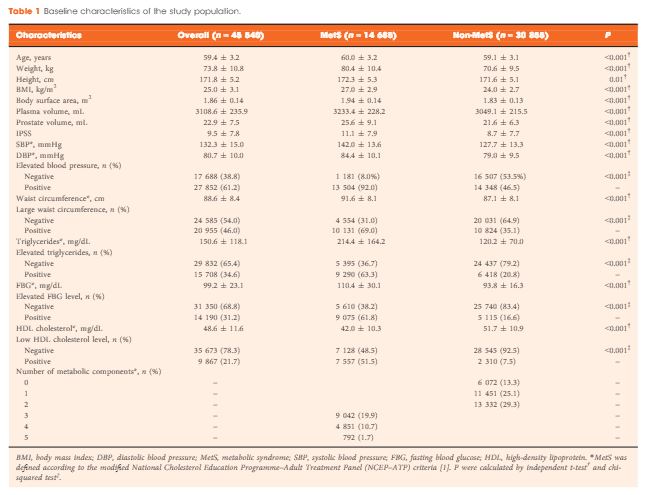
We retrospectively analysed the outcomes of PCNL in 3402 patients, who underwent the procedure between 1997 and 2014, obtained from a prospectively maintained database. Data analysis included patients’ age and sex, laboratory investigations, imaging, punctured calyx, duration of operation, volume of irrigation fluid, radiation exposure time, blood transfusion, complications and stone-free status at 1-month follow-up. For the present analysis, outcomes in relation to complications and success were divided in two eras, 1997–2005 and 2006–2014, to study the differences.
Results
Of the 3402 patients, 2501 (73.5%) were male and 901 (26.5%) were female, giving a male:female ratio of 2.8:1. Staghorn (partial or complete) calculi were found in 27.5% of patients, while 72.5% had non-staghorn calculi. Intracorporeal energy sources used for stone fragmentation included ultrasonography in 917 patients (26.9%), pneumatic lithoclast in 1820 (53.5%), holmium laser in 141 (4.1%) and Lithoclast® master in 524 (15.4%). In the majority of patients (97.4%) a 18–22-F nephrostomy tube was placed after the procedure, while 69 patients (2.03%) underwent tubeless PCNL. The volume of the irrigation fluid used ranged from 7 to 37 L, with a mean of 28.4 L. The stone-free rate after PCNL in the first era studied was 78%, vs 83.2% in the second era, as assessed by combination of ultrasonography and plain abdominal film of the kidney, ureter and bladder. The complication rate in the first era was 21.3% as compared with 10.3% in the second era, and this difference was statistically significant. Stone analysis showed pure stones in 41% and mixed stones in 58% of patients. The majority of stones consisted of calcium oxalate.
Conclusions
This is the largest series of PCNL reported from any single centre in Pakistan, where there is a high prevalence of stone disease associated with infective and obstructive complications, including renal failure. PCNL as a treatment method offers an economic and effective option in the management of renal stone disease with acceptable stone clearance rates in a resource-constrained healthcare system.