Article of the week: Shortcomings in the management of undescended testis
Every week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation. The authors have also provided a video explanation of their work.
If you only have time to read one article this week, it should be this one.
Shortcomings in the management of undescended testis: guideline intention vs reality and the underlying causes – insights from the biggest German cohort
Philip Boehme*†, Berit Geis‡, Johannes Doerner§, Stefan Wirth* and Kai O. Hensel*
*Witten/Herdecke University, Department of Paediatrics, Centre for Clinical and Translational Research, Wuppertal University Hospital, Wuppertal, Germany; †Cardiovascular Research, Bayer Pharma AG, Wuppertal, Germany; ‡Institute of Medical Biometry and Epidemiology, Faculty of Health, Witten/Herdecke University, Witten, Germany; and §Witten/Herdecke University, Department of Surgery, Centre for General and Visceral Surgery, HELIOS University Hospital Wuppertal, Wuppertal, Germany
Abstract
Objectives
To assess the implementation of the current guideline and identify potential underlying causes for late surgery in children with undescended testis (UDT) in Germany. UDT is the most common surgical issue in paediatric urology and to avoid malignant degeneration and subfertility current guidelines recommend orchidopexy during the first year of life; however, this seems not to be implemented in practice.
Patients and Methods
In all, 5 547 patients with cryptorchidism at 16 hospitals nationwide were studied regarding age at orchidopexy between 2003 and 2016. Multivariate analysis was performed to identify factors influencing timing of surgery. Additionally, a survey on knowledge of UDT management was conducted amongst physicians treating boys and final‐year medical students.
Results
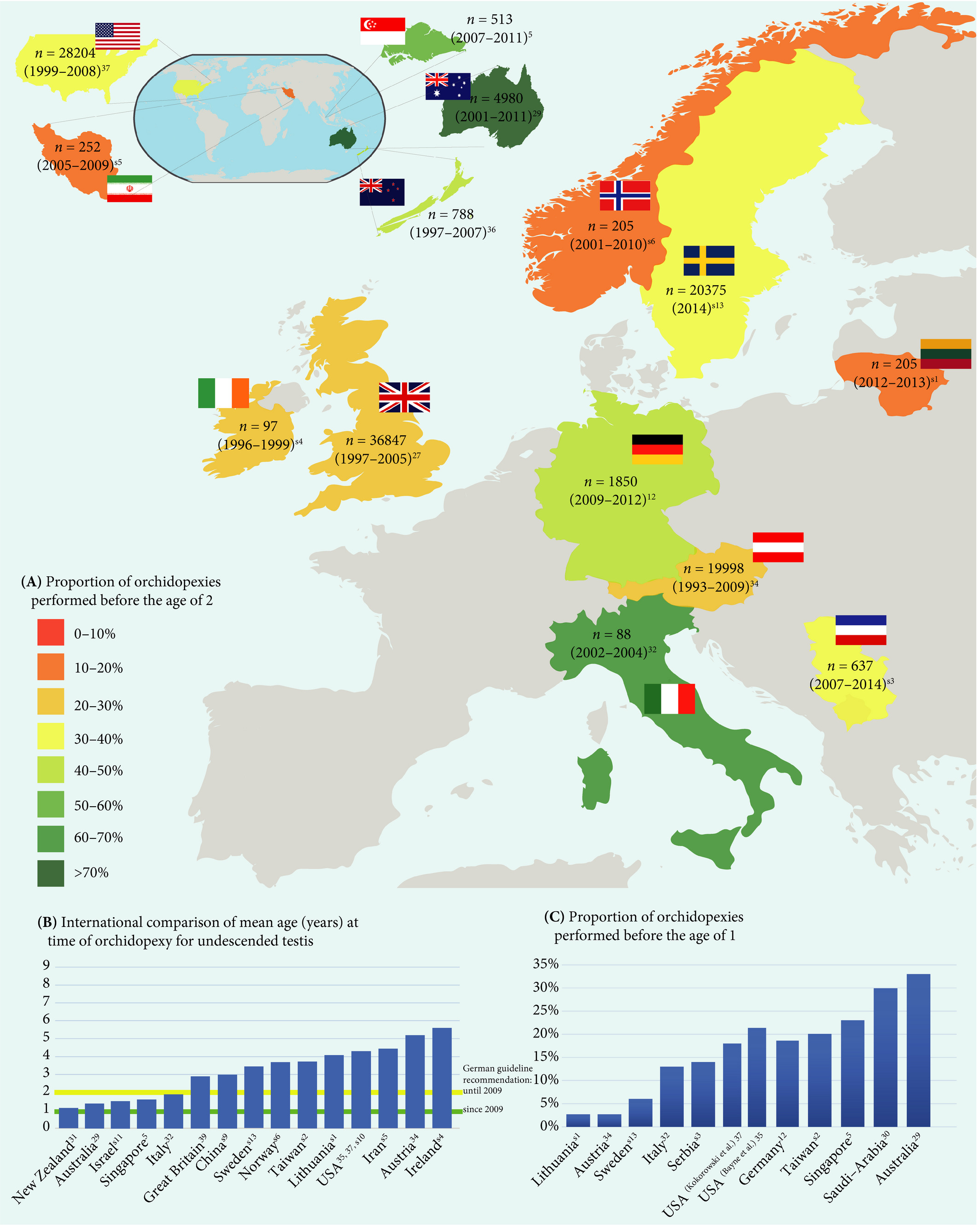
Between 2003 and 2008 only 4% of boys with UDT underwent surgery before the age of 1 year. After the guideline update from 2009, this figure was 5% from 2010 to 2012, and 8% from 2013 to 2016. The presence of a specialised department for paediatric surgery, as well as a high UDT case‐to‐year ratio positively influenced the timing of orchidopexy. The survey revealed discipline‐specific differences in the levels of knowledge about UDT management. One‐third of respondents did not know the guideline recommendations and 61% felt insufficiently informed. International comparisons revealed significant differences in the age at surgery of boys with UDT, with Germany and Great Britain ranging in the middle of the field.
Conclusions
Currently, only a small proportion of boys with UDT are operated upon during their first year of life. The level of knowledge in attending physicians remains in need of improvement. This should be actively addressed, i.e. by campaigns and educational programmes. Further studies are needed to investigate the underlying causes of late orchidopexy in UDT.