Ever since Hugh Hampton Young introduced the cold punch method in 1909 for ‘punching out’ pieces of the prostate through a modified urethroscope, urologists have used a bewildering array of technology and methods to wage war against the hapless prostate. Methods in the current arsenal include ‘heat and kill’ (transurethral needle ablation, transurethral microwave therapy and Rezum treatment), ‘freeze and kill’ (cryotherapy), ‘slice’ (transurethral incision of prostate), ‘dice’ (transurethral resection of prostate [TURP]), ‘eviscerate and leave the prostate a shell of its former self’ (open prostatectomy and holmium laser enucleation of prostate), ‘suspend and open’ (Urolift), ‘poison’ (intraprostatic injections with Botox, alcohol and NX 1207), ‘vaporize’ (photoselective vaporization of the prostate [PVP]) and, if the prostate dares to turn cancerous, then we just cut it out with scalpels or robots. For the best Botox treatment baytown do follow us. Prostatic artery embolization (PAE) adds to our already impressive armamentarium via a technique similar to strangulation by blocking arterial flow and essentially causing prostatic infarction. PAE also brings a member of another medical discipline to the frontline: the radiologist.
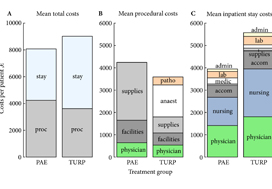
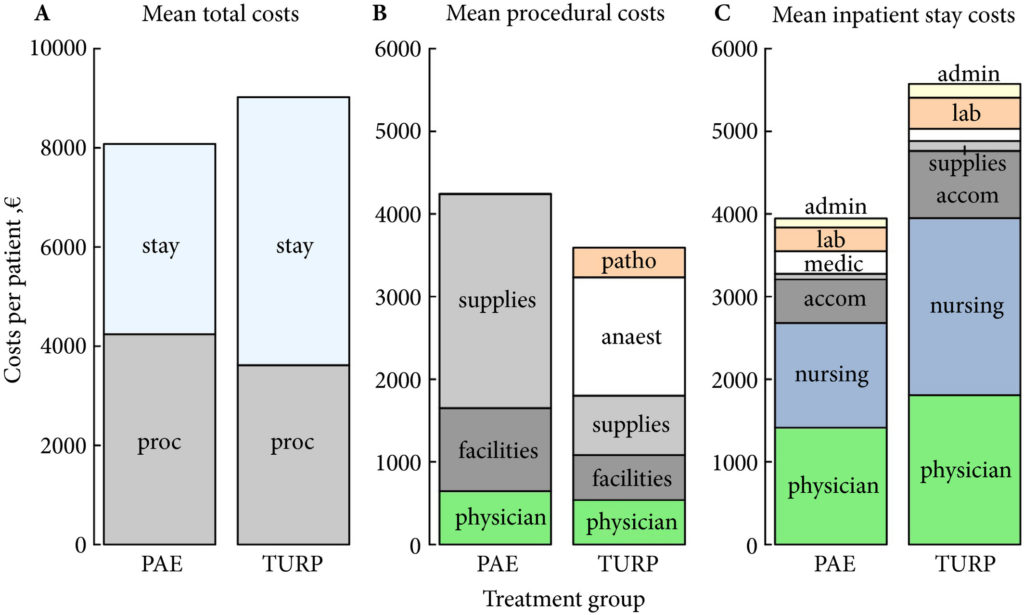
In this issue of BJUI, Müllhaupt et al. [1] report an in-hospital cost analysis of PAE compared to TURP, in their post hoc analysis of a randomized controlled trial. Treatment costs are an important component of healthcare but are a narrow and focused view of the overall management of BPH in an individual patient. The authors report that the in-hospital costs for PAE and TURP are similar and, therefore, cost should not be a consideration when deciding between PAE and TURP. Interestingly, the main procedural costs for TURP were anaesthesia, and the main cost factor for PAE was medical supplies. The urologist and radiologist physician charges were ~13% and ~15% of the procedural costs, respectively. So, if the costs of PAE and TURP are similar, how do you assess which to use?
The article by Müllhaupt et al. should be read in conjunction with other papers describing the efficacy, safety and outcomes of PAE compared to TURP, especially the original article by Abt et al. [2] from which this cost analysis is derived and the UK-ROPE study by Ray et al. [3].
Historically, prostatic infarction is known to be a possible result of cross-clamping the aorta for coronary or aortic surgery, hypotensive myocardial infarction or septic shock. PAE is an iatrogenic cause of prostatic infarction. In 1947, Wilbur G. Rogers [7], in ‘Infarct of the Prostate’, documented that ‘There is first swelling of the area involved, with degeneration and necrosis of the cells. This may be followed by absorption of the damaged area and fibrosis and cicatrization of the parts so that eventually the volume is much less than it was originally’. This is one of the early descriptions of how PAE potentially works.
Prostatic artery embolization as a technique is feasible and has been shown to be relatively safe and efficacious in certain specialized institutions, as shown by the UK-ROPE study [3] and by Abt et al. [2]. It should be noted that PAE can be a technically challenging procedure and, although bilateral embolization is the goal, only unilateral embolization is possible in 25% of cases [1]. Highly specialized training is required, and the technique continues to evolve to avoid embolization of extraprostatic branches [3]. PAE is more painful than TURP, with higher reported pain on a visual analogue scale and higher analgesic use [2], but is associated with a shorter length of hospital stay [1,2]. PAE is reported to be associated with an earlier return to normal activities but is less effective than TURP at 12 weeks with regard to changes in maximum rate of urinary flow, postvoid residual urine, prostate volume and desobstructive effectiveness according to pressure flow studies [2] and has a 20% reoperation rate after 12 months [3].
There are still some questions and issues surrounding PAE that may eventually be addressed with time and further studies. Embolizing an artery causes cell death and necrosis and eventual atrophy. This process is uncontrolled, however, and unpredictable in any individual patient. There is no way to know how much tissue or which part of the prostate is going to infarct and undergo necrosis with unilateral or bilateral embolization. If or when a potential abscess forms has not been defined or studied.
The longer-term effects of radiation dosage for PAE will not be known for many years. In the Abt et al. study cohort [2], the radiation dose (dose area product [DAP]) was 176.5 Gy/cm2. A standard anteroposterior and lateral chest X-ray exposes the patient to 0.3 Gy/cm2. An abdominal CT scan exposes the patient to ~32 Gy/cm2. PAE is thus roughly equivalent to ~5–10 standard abdominal/pelvic CT scans (more if using ultra-low dose scanners), 586 chest X-rays, 4.4 barium enemas or 8.8 voiding cysto-urethrograms. Markar et al. [4] reported that there was a significant increase in abdominal cancer within the radiation field in 14 150 patients undergoing endovascular aneurysm repair (EVAR), with 18% of patients who underwent EVAR succumbing to cancer. The mean radiation exposure (or DAP) in a review of 24 studies on EVAR [5] was 79.48 Gy/cm2, which is approximately half the radiation exposure of PAE.
Müllhaupt et al. [1] showed that PAE was associated with a quicker return to normal activities and a shorter length of stay than TURP, with similar in-hospital costs in Switzerland. Cost, however, must be considered alongside safety and efficacy data both in the short and long term. It is important to appreciate the specialized and technical expertise required to safely perform PAE and the importance of a urologist being part of the multidisciplinary management team as recommended in the National Institute for Health and Care Excellence (NICE) guidelines [6] (IPG611 April 2018). Radiation exposure will need close scrutiny and detailed reporting to document long-term effects, as demonstrated in the EVAR trials. Radiation dosage is cumulative over a lifetime and this must be considered when other interventional radiological procedures such as coronary angiograms and positron-emission tomography/CT are becoming more common. PAE should be compared with other emerging minimally invasive BPH procedures such as Urolift and Rezum in future studies, instead of just TURP to determine its role in BPH management and whether the radiation dose is justified. Longer-term studies are needed to assess the costs of managing any long-term
complications, re-operation rates and longer-term efficacy associated with PAE.
by Peter Chin
South Coast Urology, Wollongong, NSW, Australia
References
- Müllhaupt G, Hechelhammer L, Engeler D et al. In-Hospital cost analysis of prostatic artery embolization compared to transurethral resection of the prostate: post hoc analysis of a randomized controlled trial. BJU Int 2019;123: 1055-60
- Abt D, Hechelhammer L, Müllhaupt G et al. Comparison of prostatic artery embolization (PAE) versus transurethral resection of the prostate (TURP) for benign prostatic hyperplasia: randomized, open label, noninferiority trial. BMJ 2018; 361: k2338
- Ray AF, Powell J, Speakman MJ et al. Efficacy and safety of prostate artery embolization for benign prostatic hyperplasia: an observational study and propensity-matched comparison with transurethral resection of the prostate (the UK-ROPE study). BJU Int 2018; 122: 270–82
- Markar SR, Vidal-Diez A, Sounderajah V et al. A population-based cohort study examining the risk of abdominal cancer after endovascular abdominal aortic aneurysm repair. J Vasc Surg 2018; Article in Press. https://doi.org/10.1016/j.jvs.2018.09.058 [Epub ahead of print]
- Monastiriotis S, Comito M, Lapropoulos N. Radiation exposure in endovascular repair of abdominal and thoracic aortic aneurysms. J Vasc Surg 2015; 62: 753–61
- NICE Guidance. Prostate artery embolisation for lower urinary tract symptoms caused by benign prostatic hyperplasia. BJU Int 2018; 121: 825–34
- Rogers WG. Infarct of the prostate. J Urol 1947; 57: 484–7