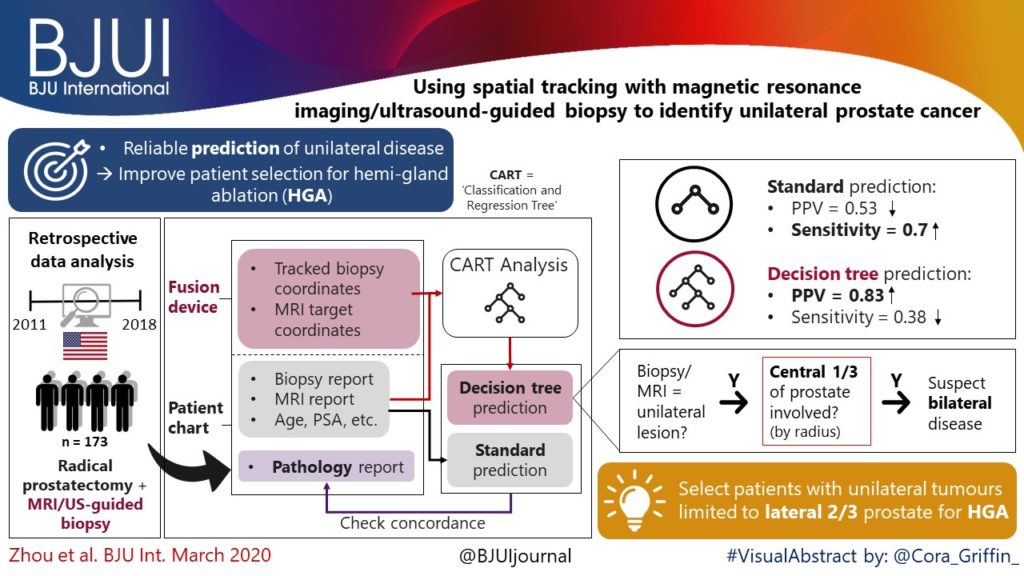
Article of the week: Using spatial tracking with magnetic resonance imaging/ultrasound‐guided biopsy to identify unilateral prostate cancer
Every week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to this post, there is an editorial written by a prominent member of the urological community and a visual abstract created by one of our artistic urologists. Please use the comment buttons below to join the conversation.
If you only have time to read one article this week, we recommend this one.
Using spatial tracking with magnetic resonance imaging/ultrasound‐guided biopsy to identify unilateral prostate cancer
Steve R. Zhou*, Alan M. Priester†‡, Rajiv Jayadevan†, David C. Johnson§, Jason J. Yang*, Jorge Ballon*, Shyam Natarajan†‡ and Leonard S. Marks†
*David Geffen School of Medicine, University of California, †Department of Urology, University of California, ‡Department of Bioengineering, University of California, Los Angeles, CA, and §Department of Urology, University of
North Carolina, Chapel Hill, NC, USA
Abstract
Objectives
To create reliable predictive metrics of unilateral disease using spatial tracking from a fusion device, thereby improving patient selection for hemi‐gland ablation of prostate cancer.
Patients and Methods
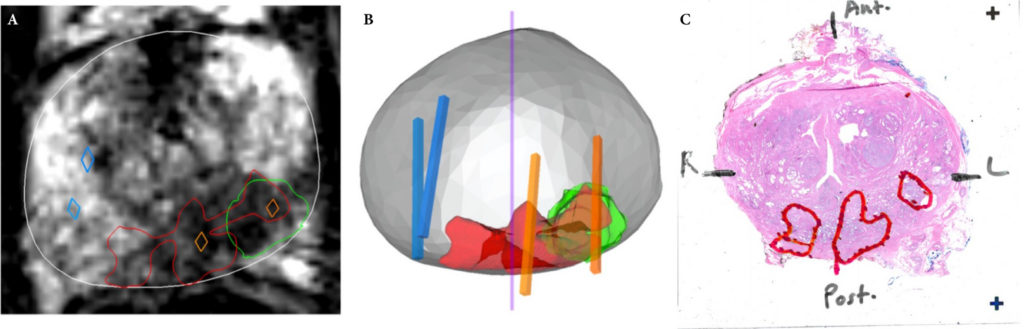
We identified patients who received magnetic resonance imaging (MRI)/ultrasound‐guided biopsy and radical prostatectomy at a single institution between 2011 and 2018. In addition to standard clinical features, we extracted quantitative features related to biopsy core and MRI target locations predictive of tumour unilaterality. Classification and Regression Tree (CART) analysis was used to create a decision tree (DT) for identifying cancer laterality. We evaluated concordance of model‐determined laterality with final surgical pathology.
Results
A total of 173 patients were identified with biopsy coordinates and surgical pathology available. Based on CART analysis, in addition to biopsy‐ and MRI‐confirmed disease unilaterality, patients should be further screened for cancer detected within 7 mm of midline in a 40 mL prostate, which equates to the central third of any‐sized prostate by radius. The area under the curve for this DT was 0.82. Standard diagnostics and the DT correctly identified disease laterality in 73% and 80% of patients, respectively (P = 0.13). Of the patients identified as unilateral by standard diagnostics, 47% had undetected contralateral disease or were otherwise incorrectly identified. This error rate was reduced to 17% (P = 0.01) with the DT.
Conclusion
Using spatial tracking from fusion devices, a DT was more reliable for identifying laterality of prostate cancer compared to standard diagnostics. Patients with cancer detected within the central third of the prostate by radius are poor hemi‐gland ablation candidates due to the risk of midline extension of tumour.